In anticipation of World Cancer Day, the International Agency for Research on Cancer (IARC), the cancer agency of the World Health Organization (WHO), disclosed the most recent global cancer burden estimates. WHO additionally presented survey findings from 115 countries, indicating that a significant number of nations fail to sufficiently fund essential cancer and palliative care services in alignment with the principles of universal health coverage (UHC).
The latest estimates from the International Agency for Research on Cancer (IARC), utilizing the most reliable data sources from countries in 2022, underscore the escalating burden of cancer, particularly its disproportionate impact on underserved populations.
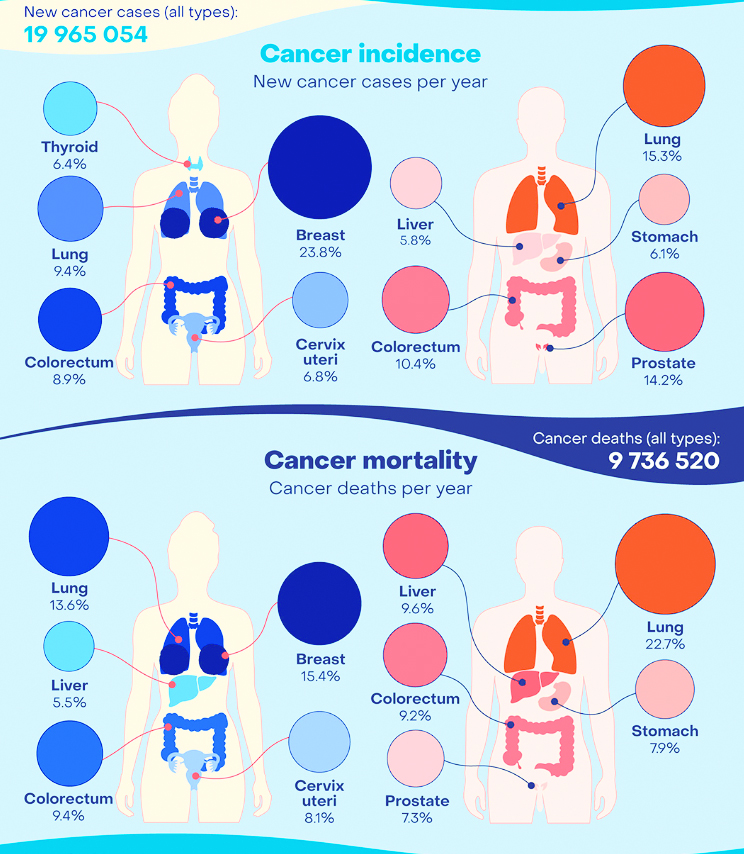
The report stated, “In 2022, there were an estimated 20 million new cancer cases and 9.7 million deaths. The estimated number of people who were alive within 5 years following a cancer diagnosis was 53.5 million. About 1 in 5 people develop cancer in their lifetime, approximately 1 in 9 men and 1 in 12 women die from the disease.”
The WHO’s global survey on Universal Health Coverage (UHC) and cancer reveals that merely 39% of surveyed countries incorporated fundamental cancer management in their funded essential health services for all citizens, known as ‘health benefit packages’ (HBP). Furthermore, only 28% of these countries extended coverage to include palliative care for individuals in need, encompassing general pain relief, not exclusively tied to cancer.
Three major cancer types: lung, breast and colorectal cancers
As per the new estimates available on IARC’s Global Cancer Observatory, 10 types of cancer collectively comprise around two-thirds of new cases and deaths globally in 2022.
Lung cancer was the most commonly occurring cancer worldwide, female breast cancer ranked second, followed by colorectal cancer, prostate cancer, and stomach cancer.
Lung cancer was the leading cause of cancer death, followed by colorectal cancer, liver cancer, breast cancer and stomach cancer.
Gender disparities were observed in both cancer incidence and mortality rates globally.
Breast cancer stood out as the most frequently diagnosed cancer and primary cause of cancer-related deaths among women, while lung cancer held this position for men. Breast cancer was predominant in the majority of countries (157 out of 185) for women.
Among men, prostate and colorectal cancers ranked as the second and third most prevalent cancers, with liver and colorectal cancers as the second and third leading causes of cancer-related deaths. For women, lung and colorectal cancers ranked as the second and third most common cancers in both new cases and deaths.
Cervical cancer, with 661,044 new cases and 348,186 deaths, occupied the eighth position globally in terms of occurrence and ninth in cancer-related mortality. Notably, it is the most prevalent cancer among women in 25 countries, predominantly in sub-Saharan Africa.
Striking cancer inequity by Human Development Index (HDI)
Global estimates expose significant disparities in the cancer burden based on human development levels, notably evident in breast cancer. In countries with very high Human Development Index (HDI), 1 in 12 women face a breast cancer diagnosis during their lifetime, with 1 in 71 succumbing to it.
In contrast, low HDI countries report a lower incidence, with one in 27 women diagnosed with breast cancer but a higher mortality rate, where one in 48 women die from the disease.
“Women in lower HDI countries are 50% less likely to be diagnosed with breast cancer than women in high HDI countries, yet they are at a much higher risk of dying of the disease due to late diagnosis and inadequate access to quality treatment,” explains Dr Isabelle Soerjomataram, Deputy Head of the Cancer Surveillance Branch at IARC.
WHO’s global survey of Health Benefit Packages (HBPs) uncovered substantial global disparities in cancer services. Notably, lung cancer-related services were reported to be 4–7 times more likely to be part of an HBP in high-income countries compared to lower-income counterparts.
On average, high-income countries were four times more likely to include radiation services in their HBPs than lower-income countries. The most significant contrast was observed in stem-cell transplantation, with a staggering 12-fold greater likelihood of inclusion in the HBP of high-income countries compared to lower-income nations.
Projected cancer burden increase in 2050
A stark projection anticipates over 35 million new cancer cases in 2050, marking a staggering 77% surge from the estimated 20 million cases in 2022. This rapid escalation in the global cancer burden is attributed to the dual impact of population ageing, growth, and alterations in people’s exposure to risk factors.
Socioeconomic development is a key contributor to this trend. The rising incidence of cancer is closely linked to factors such as tobacco use, alcohol consumption, and obesity, while air pollution remains a prominent driver of environmental risk factors.
Regarding the absolute burden, high Human Development Index (HDI) countries are projected to witness the most substantial increase in cancer incidence, anticipating an additional 4.8 million new cases in 2050 compared to the 2022 estimates.
However, the most remarkable proportional increase in incidence is expected in low HDI countries, with a staggering 142% surge, followed by medium HDI countries with a 99% increase. In addition to this, the cancer mortality in these countries is also projected to almost double in 2050.
“The impact of this increase will not be felt evenly across countries of different HDI levels. Those who have the fewest resources to manage their cancer burdens will bear the brunt of the global cancer burden,” says Dr Freddie Bray, Head of the Cancer Surveillance Branch at IARC.
“Despite the progress that has been made in the early detection of cancers and the treatment and care of cancer patients–significant disparities in cancer treatment outcomes exist not only between high and low-income regions of the world but also within countries. Where someone lives should not determine whether they live. Tools exist to enable governments to prioritise cancer care, and to ensure that everyone has access to affordable, quality services.
This is not just a resource issue but a matter of political will,” says Dr Cary Adams, head of UICC – Union for International Cancer Control.