

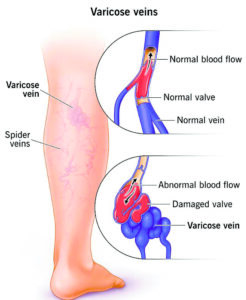
Varicose veins are a common vascular condition characterized by swollen blood vessels visible just beneath the surface of the skin, typically in the lower body. They occur when the walls of veins weaken, causing blood to pool and resulting in the appearance of blue and purple bulges on the legs, feet, or ankles. While varicose veins are often considered a cosmetic concern, they can also cause discomfort and lead to complications if left untreated.
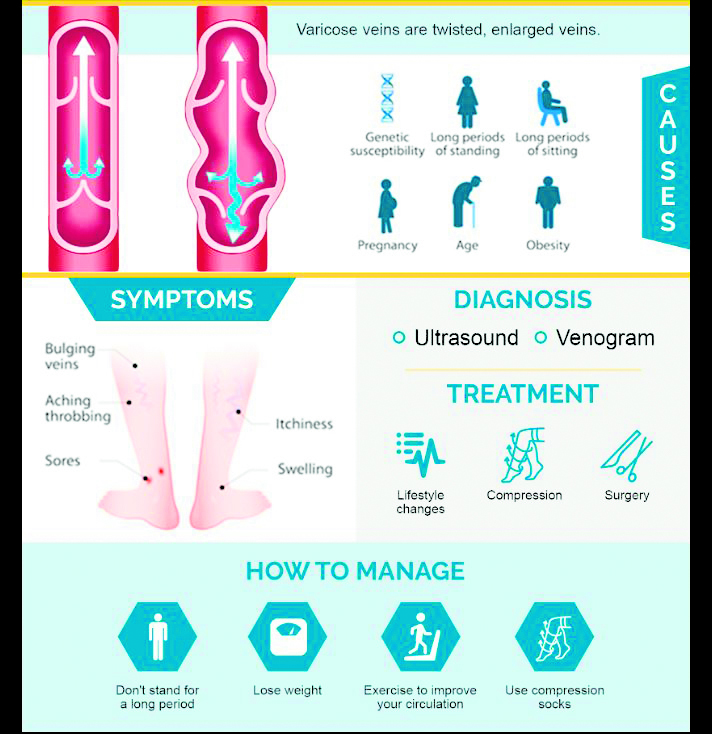
Several risk factors contribute to the development of varicose veins, including age, gender (particularly in women aged 50 or older), family history, obesity, pregnancy (especially multiple pregnancies), lack of exercise, prolonged periods of standing or sitting, and smoking. These factors can weaken vein walls and impair valve function, leading to venous insufficiency and the formation of varicose veins.
Symptoms of varicose veins may include heaviness and swelling around the ankles, leg pain, night cramps, knotty veins, changes in skin color, and the development of sores. These symptoms can vary in severity and may worsen over time if not addressed.
The underlying cause of varicose veins is related to the increased pressure on the veins in the lower body, particularly the legs, which must work against gravity to pump blood back to the heart. Weak or damaged valves within the veins can result in blood pooling and vein enlargement.
Diagnosis of varicose veins typically involves a physical examination and may include imaging tests such as a venous Doppler ultrasound of the leg. This non-invasive procedure uses sound waves to evaluate blood flow through the veins and identify any abnormalities, such as blood clots or valve dysfunction.
Treatment options for varicose veins aim to alleviate symptoms, improve circulation, and reduce the appearance of the affected veins. These may include:
1. Ultrasound-guided foam sclerotherapy (UGFS): This procedure involves injecting a foam medication into the varicose vein, causing it to shrink or disappear over time.
2. Coil embolization: In this procedure, a catheter is inserted into the varicose vein, and a platinum coil is placed inside the vein to block blood flow. Alcohol is then injected to destroy the vein.
3. Surgical vein stripping: This surgical procedure involves tying off and removing the affected vein through small incisions in the skin.
4. Ambulatory phlebectomy: This surgical technique involves removing varicose veins through small incisions in the skin using specialized hooks.
5. Endovenous laser treatment (EVLT) or endovenous laser ablation therapy (EVLA): This minimally invasive procedure uses a laser fiber inserted into the varicose vein to heat and collapse the vein, causing it to shrink and disappear.
6. Radiofrequency ablation (RFA): In this procedure, radiofrequency waves are used to heat and close off the varicose vein.
Overall, treatment for varicose veins should be tailored to individual patient needs and preferences, with consideration given to the severity of symptoms, the presence of complications, and overall health status. By addressing both symptoms and underlying causes, patients can experience improved quality of life and reduced risk of complications associated with varicose veins.
The author is the Hon. Consultant Endovascular Surgery, PSRI Hospital, New Delhi.