The human body has been seen as a tightly woven tapestry, with organs playing distinct roles in a grand physiological orchestra. But beneath the surface, a hidden chorus of trillions sings a vital melody: the gut microbiota. These microscopic maestros, residing within our intestines, are not mere bystanders; they are active conductors, influencing our health in ways we are only beginning to understand. And in the complex dance of diabetes, their role is proving to be both profound and intricate.
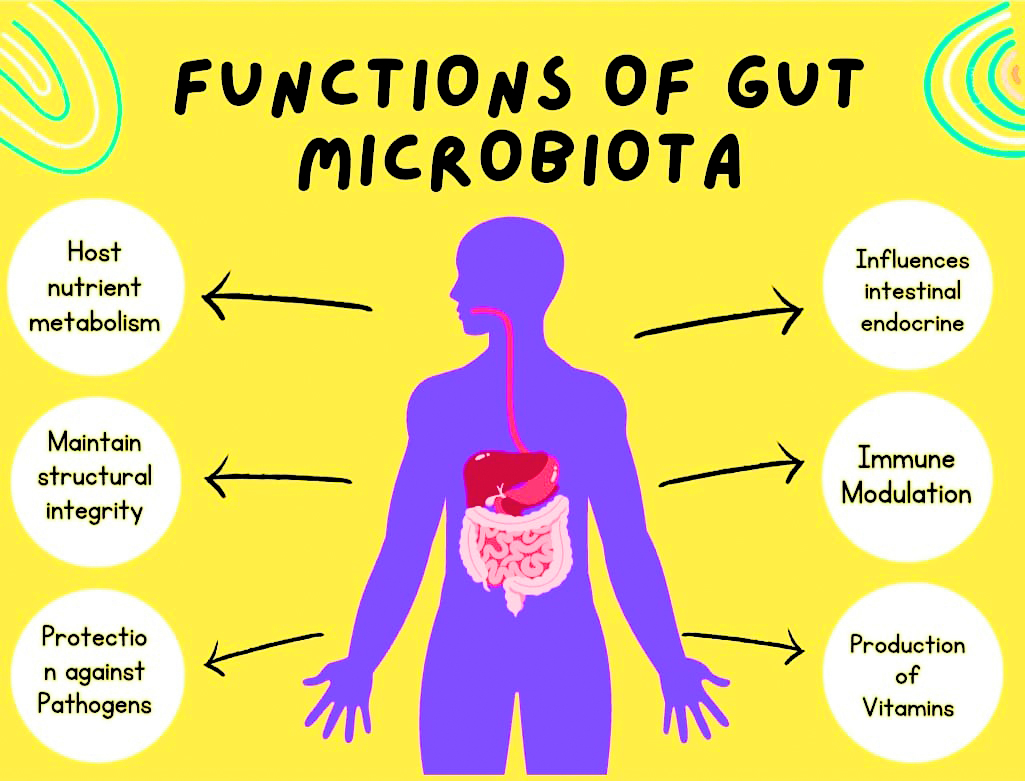
Diabetes, a metabolic illness defined by elevated blood sugar levels, has long been related to factors such as heredity and lifestyle. Recent study, however, has revealed an unexpected guest player in this drama: the gut flora. Studies have revealed a significant variation in the composition of gut bacteria between those with and without diabetes. This shows that when the microbial symphony is out of tune, it can contribute to the development and progression of this chronic disease. So, how do these tiny maestros conduct the diabetic dance? Their influence is multifaceted, operating through a series of intricate mechanisms.
1. Metabolic Mayhem: Our gut bacteria are like small factories, producing a variety of substances that affect our metabolism. Beneficial bacteria create short-chain fatty acids (SCFAs), which affect insulin sensitivity and glucose absorption. However, in diabetes, the generation of these beneficial SCFAs may be interrupted, resulting in poor glucose management.
2. Inflammatory Interlude: Gut bacteria are also important in regulating inflammation. Pro-inflammatory chemicals can be generated when the microbial balance is disrupted, resulting in chronic low-grade inflammation. This inflammation, in turn, can compromise insulin signaling and contribute to diabetes development.
3. Breakdown of the Gut Lining: The gut lining serves as a barrier, preventing dangerous substances from entering the bloodstream. In diabetes, however, this barrier can become leaky, allowing bacterial compounds to enter the body and aggravate inflammation. The gut microbiota can alter the barrier’s integrity, providing another layer to the complicated interplay.
4. Hormonal Balance: Gut bacteria also influence hormone production, which regulates hunger, fullness, and digestion. Diabetes can interrupt this hormonal symphony, resulting in weight gain and subsequent metabolic abnormalities.
Understanding the role of the gut microbiota in diabetes opens up exciting avenues for therapeutic interventions. Probiotics, prebiotics, and even fecal microbiota transplantation are being explored as potential ways to modulate the gut orchestra and restore balance. By harmonizing the microbial melody, we may be able to conduct a new kind of dance – one where diabetes loses its grip on our health.
However, it is important to remember that this is still a young field of research. While the evidence is promising, more studies are needed to fully understand the complex interplay between the gut microbiota and diabetes. Nevertheless, the gut symphony is captivating researchers and offering a new perspective on this chronic disease. By listening closely to the chorus of microbes within, we may finally find the key to turning the tide on diabetes and dancing towards a healthier future.
The author is Senior Consultant in Endocrinology at Indraprastha Apollo Hospital, New Delhi.