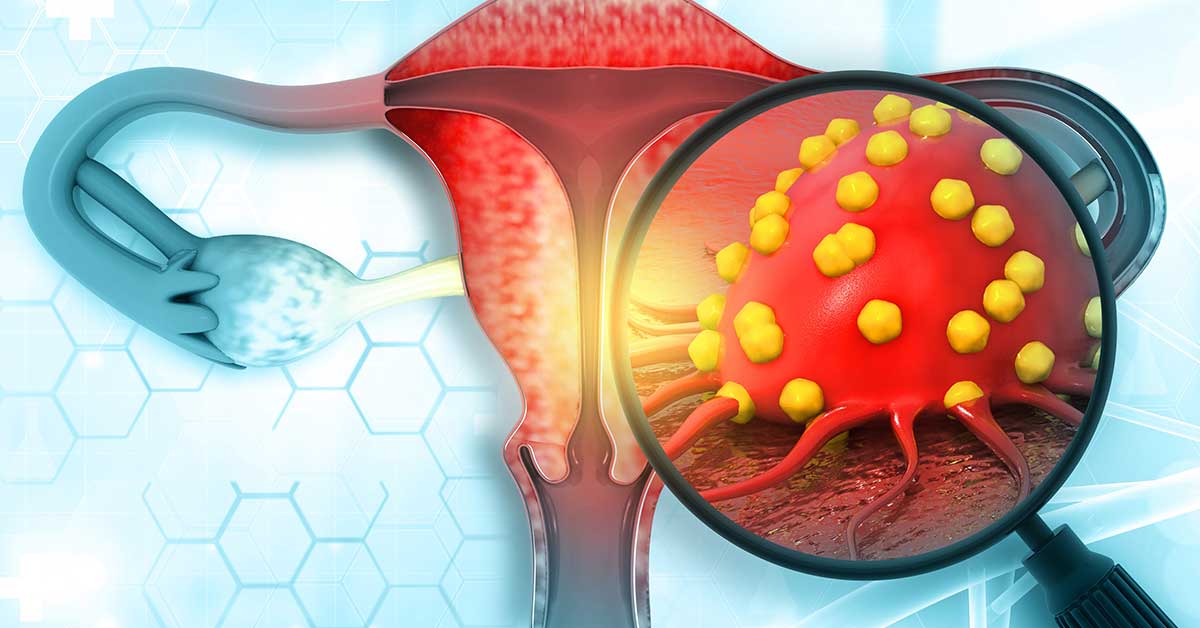
Ovarian cancer remains one of the most deadly forms of cancer worldwide, with its high mortality rates placing it as the fifth most common cause of cancer death among women. Despite significant progress in the understanding of ovarian cancer and its treatment over the years, the disease continues to present major challenges to both researchers and healthcare providers globally. Recent advancements in molecular research, coupled with epidemiological data from various parts of the world, have highlighted shifting trends in ovarian cancer incidence. These trends vary across regions, with different subtypes of ovarian cancer being more prevalent in certain geographical areas than others. A global study analyzing these changes sheds light on the evolving patterns of ovarian cancer, providing critical insights that could shape future research and improve prevention and treatment strategies.
This article will delve into the findings of a major global study on ovarian cancer, exploring the changing patterns of incidence by cancer subtype and region. It will examine how factors like genetics, lifestyle, environment, and healthcare access contribute to these trends, and how early detection and personalized treatment may hold the key to improving outcomes for women with ovarian cancer.
Ovarian cancer is a complex disease that arises from the ovaries, the female reproductive organs responsible for producing eggs and hormones such as estrogen and progesterone. There are several types of ovarian cancer, but they can generally be categorized into three main subtypes:
The global study examined how the incidence of each of these subtypes has changed over time and across different regions. Researchers found that while the overall global incidence of ovarian cancer has remained relatively stable in many high-income countries, the rates have shifted in low- and middle-income regions. Additionally, the relative proportions of different subtypes of ovarian cancer are changing, with some regions experiencing an increase in certain types, particularly epithelial ovarian cancer.
The study revealed important regional differences in the incidence of ovarian cancer, highlighting the role of both environmental and genetic factors in shaping these patterns. In general, the incidence of ovarian cancer is higher in developed countries compared to developing nations. However, this does not tell the whole story, as the trends vary significantly by subtype.
1. Epithelial Ovarian Cancer (EOC)
Epithelial ovarian cancer (EOC) is the most common and most studied subtype of ovarian cancer. It is often diagnosed at later stages due to its nonspecific symptoms, which makes it more difficult to treat effectively. The global study found that the incidence of EOC has been relatively stable or even declining in some high-income countries. This trend may be attributed to a variety of factors, including improved access to healthcare, advancements in early detection techniques, and changing reproductive behaviors.
For instance, the use of oral contraceptives (OCs) has been shown to reduce the risk of developing ovarian cancer, and in many high-income countries, the widespread use of OCs has led to a gradual decrease in ovarian cancer incidence over the past few decades. Additionally, women in developed countries tend to have fewer children, have them later in life, or choose to not have children at all. These reproductive choices are thought to reduce the number of ovulations and, in turn, lower the risk of ovarian cancer.
However, the situation is different in low- and middle-income countries. In these regions, the incidence of EOC has been rising, which is likely due to a combination of factors. For example, lifestyle changes associated with urbanization, such as increased consumption of processed foods, reduced physical activity, and delayed childbirth, are contributing to a higher risk of EOC. Furthermore, the lack of widespread screening and early detection programs means that many cases of ovarian cancer in these regions are diagnosed at advanced stages, making treatment more difficult and survival rates lower.
2. Germ Cell Tumors
Germ cell tumors of the ovaries are relatively rare, but they tend to occur in younger women, often affecting women in their teens or early 20s. The global study highlighted a fascinating trend: while the overall incidence of ovarian cancer has remained stable in many regions, there has been a noticeable increase in the incidence of germ cell tumors in certain regions, particularly in low-income countries.
One of the key reasons for this trend could be related to increasing survival rates of children and young adults with various medical conditions, as advances in pediatric healthcare have reduced early mortality from diseases unrelated to cancer. As more young women reach adulthood, the incidence of conditions such as germ cell tumors, which are more likely to affect women at younger ages, could be rising.
Germ cell tumors are unique because they often have a better prognosis compared to epithelial ovarian cancer, due to their responsiveness to chemotherapy and other treatments. However, the increase in their incidence, particularly in regions with limited access to specialized medical care, raises concerns about late-stage diagnoses and inadequate treatment options.
3. Sex Cord-Stromal Tumors
Sex cord-stromal tumors, though rare, have also exhibited a shift in incidence, with some regions reporting an increase in these tumors. These tumors are often less aggressive than epithelial tumors and are more likely to be diagnosed at an earlier stage. In developed countries, the incidence of these tumors appears to be steady, with healthcare infrastructure enabling more frequent diagnoses.
However, in low- and middle-income countries, the incidence of sex cord-stromal tumors appears to be on the rise. This could be due to a combination of factors, including better recognition and diagnosis, as well as improved survival rates in general. These tumors often present with hormonal symptoms, such as changes in menstrual cycles or unusual growth patterns, which can make them easier to identify and treat early.
The study also examined the impact of environmental and genetic factors on ovarian cancer trends. Researchers found that the incidence of ovarian cancer is influenced not only by lifestyle and reproductive factors but also by genetic predisposition.
In some regions, particularly those with a high prevalence of specific genetic mutations, the rate of ovarian cancer is significantly higher. For example, women with mutations in the BRCA1 and BRCA2 genes have a much higher risk of developing ovarian cancer, with studies showing that the lifetime risk for these women can be as high as 40-50%. Genetic counseling and testing are crucial for women with a family history of ovarian cancer or related cancers, as early detection and preventive measures can greatly reduce the risk of developing the disease.
In contrast, some populations in low- and middle-income countries have lower rates of ovarian cancer, possibly due to a combination of genetic resistance and limited exposure to environmental risk factors. However, as globalization continues to spread Westernized lifestyles to these regions, the rates of ovarian cancer, particularly epithelial ovarian cancer, are expected to rise.
A key finding of the global study is the growing importance of prevention and early detection in reducing the burden of ovarian cancer. Early-stage ovarian cancer is often asymptomatic or presents with vague symptoms, making it difficult to diagnose before it has spread. As a result, ovarian cancer is often diagnosed at advanced stages, when the prognosis is much poorer.
The global study stresses the need for increased investment in early detection technologies, particularly in low- and middle-income countries where access to healthcare is limited. Screening programs, such as transvaginal ultrasounds and blood tests for tumor markers, have been shown to detect ovarian cancer at an earlier stage, improving survival rates. Furthermore, education about the signs and symptoms of ovarian cancer and the importance of regular check-ups could help reduce late-stage diagnoses and improve outcomes for women.
As the study demonstrates, ovarian cancer incidence is rising in some regions, particularly among women in low- and middle-income countries. This underscores the importance of global efforts to improve ovarian cancer awareness, prevention, and treatment.
Countries and organizations are beginning to take action by investing in public health campaigns, improving healthcare access, and developing new treatment options for ovarian cancer. Governments are also pushing for better policies on genetic testing and counseling, which can help women understand their risk and take preventive action if necessary.
The global study on ovarian cancer trends provides invaluable insights into the changing patterns of the disease across different regions. As the incidence of ovarian cancer increases in many parts of the world, it is crucial to understand the role of genetic, environmental, and lifestyle factors in shaping these trends. The findings underscore the importance of early detection, personalized treatment, and global collaboration to address the growing ovarian cancer burden.
By investing in research, healthcare infrastructure, and awareness campaigns, it is possible to improve outcomes for women worldwide. The global fight against ovarian cancer requires a concerted effort to understand the evolving trends and implement strategies that can make a meaningful difference in the lives of women around the globe.