Understanding the Basics:
Childhood leukaemia, a rare disease among children, alters the DNA of white blood cells which leads to cells growing expeditiously in the body. It is the most prevalent category of paediatric cancer that originates from the bone marrow, a spongy material placed in centre of the bones responsible for engendering various blood cells. Most incidences of childhood leukaemia have an acute presentation, designating that patients show small history of consequential clinical symptoms unlike the chronic leukaemia in adults, which are mostly discovered incidentally during blood investigations.
Decoding Complexities:
Accounting for 75-80% of all childhood leukaemia cases, the most common sub-category of childhood blood cancer is Acute Lymphoblastic Leukaemia (ALL), caused by alteration in the DNA of lymphoid stem cells. However, high cure rates are also associated with the disease. While the treatment is long and demanding in all aspects, approximately 80 – 90% of children diagnosed with ALL will be able to obtain long-term remedy. However, this is attainable only if it is diagnosed early and treated as per standard contemporary treatment protocols. This is followed by the next most common category of paediatric leukaemia, Acute Myeloid Leukaemia (AML). Also known as Myeloid Leukaemia, this sub-category accounts for 15-20% of childhood leukaemia cases.
Prevalent Factors behind the Disease
As we all understand, any cancer arises due to genetic mutations in the DNA of an individual. While in most cases the mutation transpires arbitrarily in cells undergoing division, several factors have been identified in development of leukaemia. This includes a range of concerns pertaining to exposure to radiation, chemicals (such as benzene), and certain viruses. However, it is important to note that the possibility of these environmental factors and genetic mutations raising the risk of leukaemia is only miniscule. In fact, except infrequent familial leukaemia, genetic mutations resulting in childhood leukaemia are not inherited. Perhaps, an intricate interaction between genetics and environmental factors can trigger the development of leukaemia in a child. Therefore, rigorous research and colossal-scale studies are required to ascertain the real reason behind development of the disease.
Here’s The Key:
Early diagnosis can certainly pave a better and healthier future for children. However, diagnosing blood cancer in children requires a series of steps to first confirm the presence of the disease, its type, and then risk-stratify the condition to decide the ideal course of treatment:
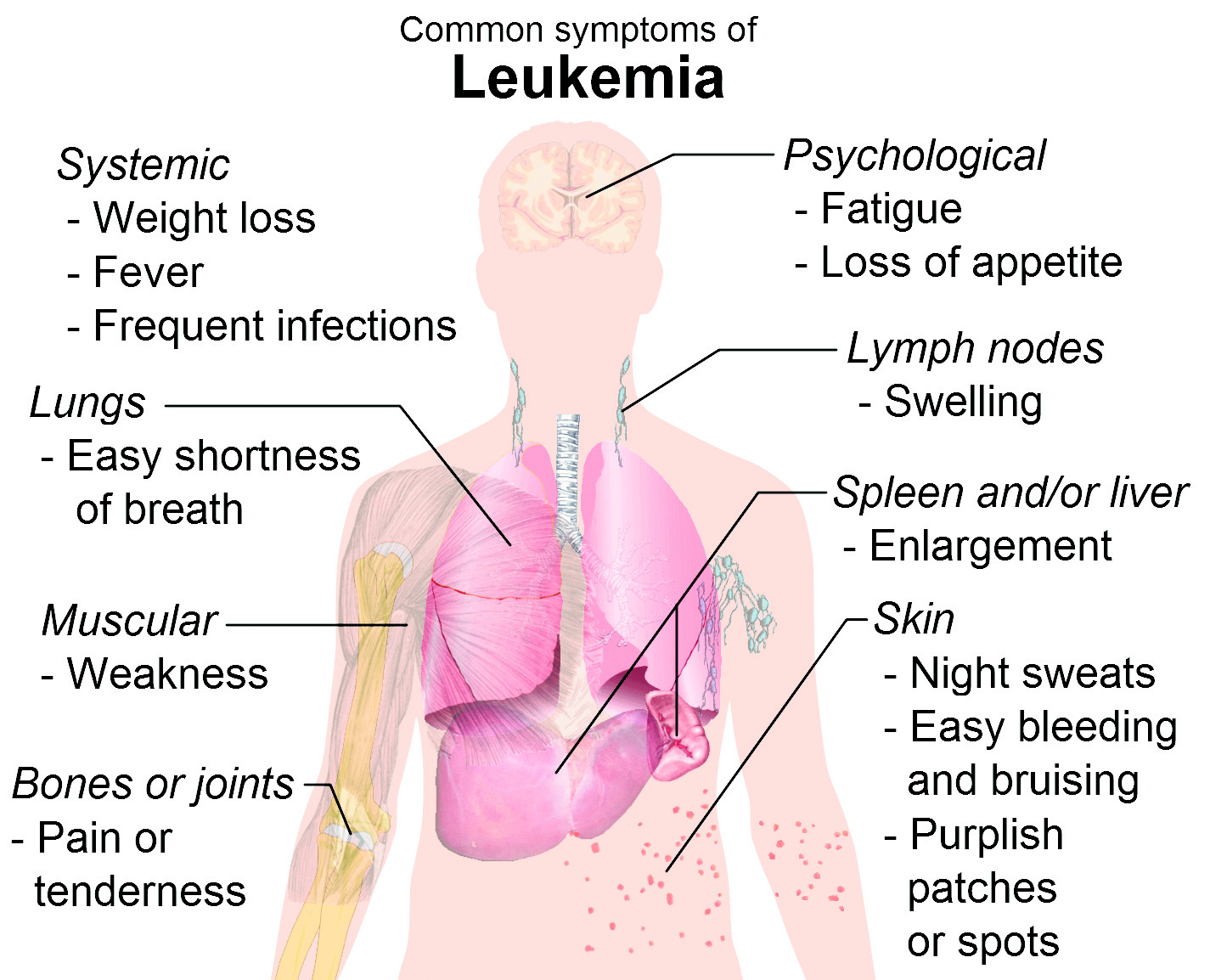
=History and Physical examination: A paediatric haemato-oncologist must record a child’s full medical history and consider symptoms a child might be experiencing at that time. For instance, a child may have easy lassitude, pale skin due to low haemoglobin, frequent unexplained pyrexia due to diseased white blood cells or spontaneous bruising due to low platelet count. As leukaemia originates in the bone marrow, generalised bone pain is also one of the common symptoms. The doctor should conduct a physical examination to check for disease signs, such as an enlarged lymph node or enlarged liver or spleen.
=Blood Tests: Abnormalities in the blood cell count or appearance may provide clues to the presence of childhood leukaemia. Most consequential blood test is a complete blood count test with a good peripheral smear. Since leukaemia is the cancer of white blood cells accompanied by low calibers of haemoglobin and platelet count, peripheral smear is additionally examined using a microscope to differentiate blasts (blood cancer cells) from normal cells.
=Bone Marrow Aspiration and Biopsy: Bone marrow aspiration and biopsy are crucial for confirming the diagnosis of blood cancer. This involves extracting a small amount of bone marrow and a tiny piece of bone from the hipbone. A haemato-pathologist examines the bone marrow sample under a microscope to look for abnormal cells. This test is done under sedation to reduce discomfort in case of children. It is a minor procedure which is conducted on a day-care basis and is not associated with any long-term side-effects.
=Flow Cytometry: The technique is primarily used to characterize the type of eccentric white blood cells in blood or bone marrow, which is instrumental in relegating the type of leukaemia (ALL vs AML).
=Cytogenetic and Molecular Testing: Oncologists often rely on molecular testing to detect concrete gene mutations, for risk stratification, as it guides the treatment decisions.
Treatment Alternatives Post-Diagnosis
While chemotherapy is opted as the main treatment for most childhood leukaemia incidences, bone marrow transplant might be required in certain high-risk cases, especially if not exhibiting anticipated response to chemotherapy. In case of Acute Lymphoblastic Leukaemia cases, the treatment can be long but rewarding, increasing possibility for a long-term cure. Additionally, with the advent of immunotherapy, long-term cure has become a reality even in refractory cases. However, timely diagnosis is mandatory for the same through close collaboration between parents, paediatricians, and paediatric haemato-oncologists.
The author is the Senior Paediatric Haemato-Oncologist, Delhi NCR.