Human papillomavirus (HPV) is a sexually transmitted pathogen that causes anogenital and oropharyngeal disease in males and females. There are various genotypes and amongst them genotype 16 and 18 causes 70 % cancer cervix and 90% anal cancers globally. Rest of the genotypes like 31,33,45 ,52 58 cause rest of 20-30% cervical cancers. HPV vaccines have been developed to prevent HPV infection and development of associated HPV related anogenital and cervical diseases.
The risk factors are as follows –
1. Multiple sexual partners and unprotected penetrative sex.
2. Contaminated Fomite, and digital/vaginal contact may also spread the virus.
It will be the imperative to consider the possibility of an underlying immune disorder in patients with particularly severe or refractory HPV infection. Human papillomavirus virus vaccine is beneficial for both females and males. In females it is most effective in prevention of cervical cancer.
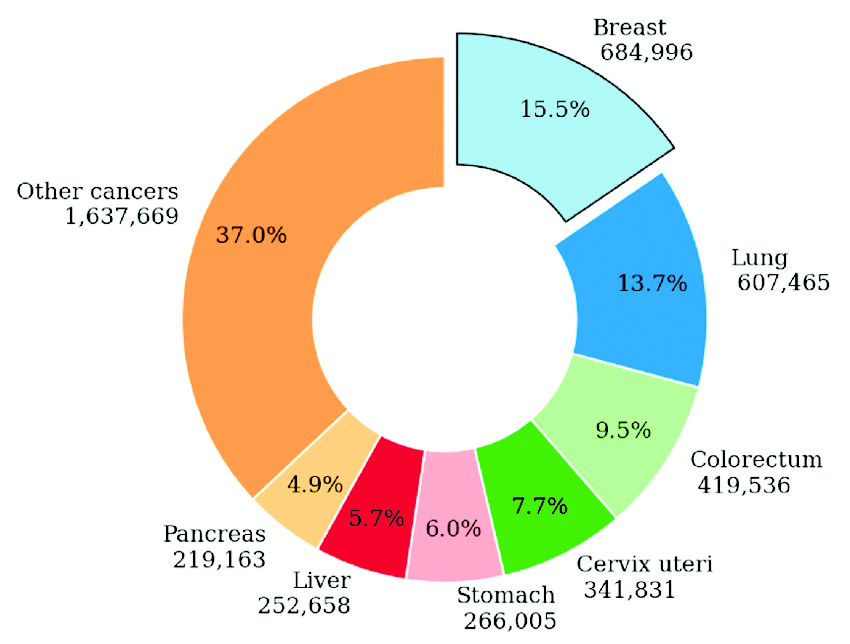
Human papilloma virus quadrivalent, or human papillomavirus bivalent vaccine provides a direct benefit to female recipients by safely protecting against cancers that can result from persistent HPV infection. This preventive effect is most notable and best studied with cervical cancer, while in males it provides direct benefit by preventing genital cancer and warts.
HPV vaccination is recommended for all females and males in the following age ranges.
• Routine HPV vaccination is recommended at 11 to 12 years age.
• Catch up vaccination is recommended for girls between 13 to 26 years.
• For adults 27 years and older, catch-up vaccination is not routinely recommended, even if they are older than 26 years.
Efficacy
HPV vaccination effectively prevents cervical disease, including cervical intraepithelial neoplasia (CIN2 or 3) and adenocarcinoma in situ. Various International studies have shown substantial decreases in cervical cancer incidence following initiation of national HPV vaccination programs. In addition, quadrivalent and 9-valent HPV vaccines have been demonstrated to reduce the incidence of vaginal and vulvar intraepithelial neoplasia. Vaccine efficacy is greatest in those who do not have prior HPV infection.
Duration of protection
HPV Vaccine has shown excellent and consistent protection against high-grade cervical, vaginal, and vulvar neoplasia at least for 10 years following vaccination. Persistent antibody levels and protection against HPV infection have also been reported up to 10 years following vaccination.
Special Population
Pregnant or breastfeeding females — HPV vaccination during pregnancy is not recommended. During Vaccination process if a lady becomes pregnant the lady should be assured that the vaccination will not have any deleterious effect on outcome of pregnancy. However, the process of vaccination should be stopped.
Lactating females can receive the immunization series since subunit vaccines do not affect the safety of infant breastfeeding.
Pre-existing HPV-associated disease — A history of genital warts, a positive HPV test result, or abnormal cervical, vaginal, vulvar, or anal cytology all indicate a prior HPV infection. Vaccination is still recommended in individuals within the recommended age range who have evidence of prior HPV infection, as it can still provide protection against infection with HPV vaccine types not already acquired.
Healthcare workers at risk for occupational exposure — There is evidence that upper aerodigestive (nasal and oropharyngeal) HPV infection may be transmitted through exposure to HPV vapors generated during surgical excision or ablation of HPV-associated lesions, although the magnitude of this risk is unknown. This class of people should also receive Vaccination.
The author is the VSM, Medical Oncologist, American Oncology Institute (AOI) Gurugram.