

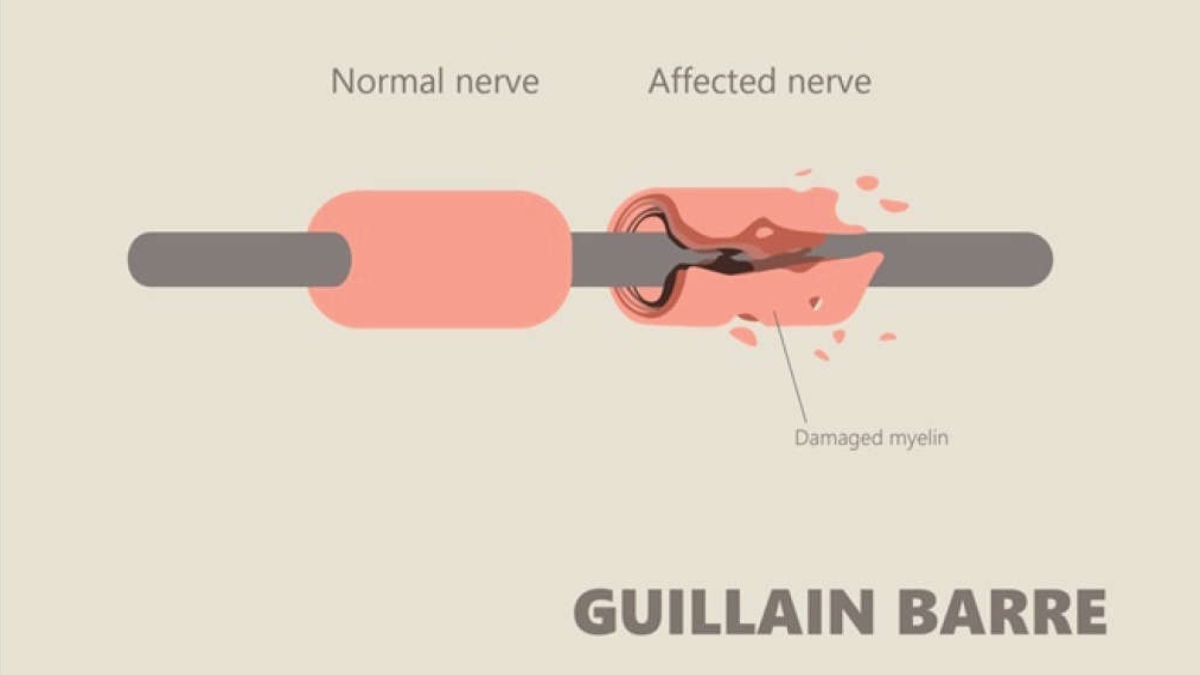
Guillain-Barré syndrome (GBS) is a rare neurological disorder in which the body’s immune system mistakenly attacks part of its peripheral nervous system, that is, the network of nerves located outside of the brain and spinal cord. From very mild cases with brief weakness to critical stages of paralysis that can cause a disability to breathe independently, patients can face a wide range of complications with GBS.



It has been observed that Guillain-Barré syndrome is a potentially serious hurdle associated with Covid-19 today. Many patients developed the GBS three weeks after testing positive for Covid-19. As Covid-19 is also a viral infection caused by a neurotropic virus, it can trigger this syndrome in a patient. The increase in Covid-19 cases has significantly resulted in many Guillain-Barré syndrome cases. People within the age group of 25 to 35, and 50 to 70 are most commonly affected.
It is essential for family members to keep a watch out for any of the symptoms.
Below are the indications:
1. Pricking or pins and needles sensations in the hands and feet
2. Instability and lack of coordination
3. Difficulty swallowing, speaking or chewing
4. Muscle twitching
5. Vision and eye muscle difficulties
6. Abnormal heartbeat/rate or blood pressure
7. Problems with digestion and/or bladder control.
As soon as a person notices any signs of Guillain-Barré syndrome, he or she should see a doctor for a definitive diagnosis. Early detection can aid in the treatment process and make it easier. A neurologist (a specialist who specialises in nervous system illnesses) will be involved in the treatment and may perform certain tests like nerve conduction studies (NCS) electromyography (EMG) that measures the electrical activity of nerves and muscles, lumbar puncture (spinal tap) and analysis of spinal fluid, along with breathing and blood tests.
1. Patients demonstrated considerable improvement after five days of IVIG treatment and plasmapheresis
2. If ventilator assistance is required, the patient must be admitted to an intensive care unit
3. It has also been observed that there is a residual disability at the time of discharge
Here is a list of do’s and don’ts if you are diagnosed with GBS:
1. Do understand that Guillain-Barré syndrome can be devastating because of its sudden and unexpected onset
2. Do realise that recovery isn’t necessarily quick. It might take a few weeks, sometimes months, or even years to recover from GBS.
3. Do call your health care provider if you notice muscle weakness
4. Do call your healthcare provider if you develop numbness or tingling feelings, have trouble swallowing or breathing, feel depressed or get a fever
5. Don’t be afraid to ask for social and emotional support
6. Don’t miss any follow-up appointments after being discharged from the hospital
It is essential for people to be aware of this syndrome as the diagnosis becomes more challenging when the patient visits the hospital at later stages for treatment. More awareness can indeed save lives.
The writer is a Consultant – Neurologist and Stroke Physician, Manipal Hospitals, Malleshwaram.