Artificial Intelligence (AI) has emerged as a groundbreaking tool in the detection of breast and ovarian cancers, with studies from Germany and Sweden providing compelling evidence of its potential to outperform traditional medical expertise. These studies, published in well-regarded scientific journals, demonstrate that AI technologies can be as effective as, or in some cases even more accurate than, radiologists and physicians in diagnosing these life-threatening conditions. The remarkable success of AI in cancer detection holds promise for transforming the way we approach cancer screening and diagnosis globally.
AI’s Role in Breast Cancer Detection
Breast cancer is one of the most common forms of cancer, affecting millions of women worldwide. Early detection through mammograms is crucial for improving survival rates, but interpreting mammograms can be challenging, even for seasoned radiologists. A study conducted in Germany, which involved nearly half a million women, assessed the impact of AI on mammogram screenings. The results were striking: AI-assisted screening led to the identification of more breast cancer cases than traditional methods.
The study revealed that when radiologists used AI to assist in interpreting mammograms, the detection rate increased significantly. Specifically, AI helped detect 6.7 breast cancer cases per 1,000 women, compared to 5.7 cases per 1,000 in the control group, which used conventional screening methods without AI assistance. This increased detection rate was achieved without a corresponding rise in false positives, a common concern with any cancer screening method. False positives can lead to unnecessary procedures, causing patient distress and additional healthcare costs. By improving accuracy and reducing the chances of false positives, AI demonstrates its potential to enhance the efficiency of mammogram screenings while maintaining high diagnostic accuracy.
Cancer epidemiologist Alexander Katalinic, who was involved in the study, emphasized the potential of AI to improve mammography outcomes. He noted that AI’s performance in breast cancer detection was on par with human doctors and radiologists, if not superior in some cases. The AI technology used in the study was able to identify cancerous tissues in mammogram images more efficiently than human counterparts, helping radiologists detect cancers earlier and more accurately. This breakthrough offers a glimpse into a future where AI is an indispensable tool in cancer screening, reducing human error and potentially saving lives through earlier intervention.
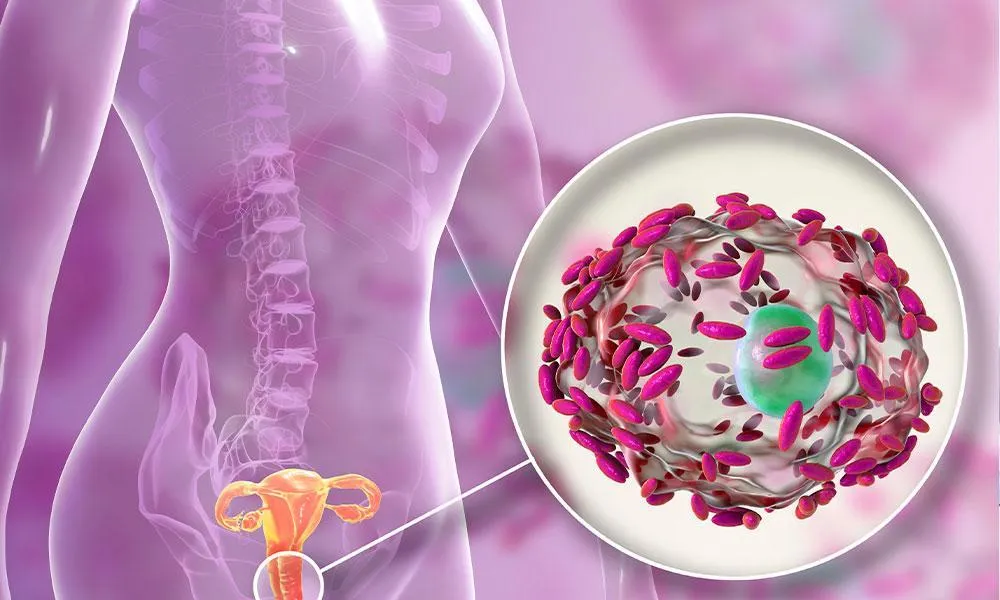
AI’s Advantage in Ovarian Cancer Detection
Ovarian cancer, though less common than breast cancer, is often diagnosed at a later stage due to the lack of clear symptoms in its early stages. This late detection contributes to its high mortality rate. Early diagnosis is critical to improving outcomes for patients, and AI is proving to be a powerful tool in this area as well. Researchers at Sweden’s Karolinska Institute have developed AI-based models that can outperform both expert and non-expert radiologists in detecting ovarian cancer in ultrasound images.
In their study, the AI models were trained on over 17,000 ultrasound images taken from 3,652 patients across 20 hospitals in eight countries. The results showed that AI outperformed human experts in identifying ovarian cancer, with the AI models achieving an accuracy of 86.3%, while expert radiologists achieved 82.6% accuracy, and non-experts only reached 77.7% accuracy. This ability to distinguish between benign and malignant ovarian lesions with high precision is crucial, as it helps avoid unnecessary surgeries and interventions that can be harmful to patients.
Ovarian lesions, which can be either benign (non-cancerous) or malignant (cancerous), often present a diagnostic challenge. AI’s ability to accurately distinguish between these lesions is a game-changer in the field of gynecological oncology. The AI models in the study were able to assess the images and classify the lesions more accurately than human experts, enabling faster and more reliable diagnoses. As ovarian cancer is often diagnosed only when it has reached an advanced stage, this technology has the potential to revolutionize early detection, allowing for timely interventions and improved survival rates.
Professor Elisabeth Epstein, a lead researcher in the study, highlighted the global shortage of ultrasound experts, particularly in rural and underserved areas. This shortage often leads to delayed diagnoses and unnecessary medical interventions. AI offers a promising solution to this problem by providing a supplementary tool that can assist or even replace human experts in some cases. By integrating AI into clinical practice, healthcare systems can alleviate the burden on overworked professionals and ensure more timely and accurate diagnoses for patients.
AI in Cancer Detection: A Global Perspective
The success of AI in detecting both breast and ovarian cancers has significant global implications. According to the World Health Organization (WHO), breast and ovarian cancers are among the leading causes of cancer-related deaths worldwide. Early detection is a key factor in improving survival rates, but access to skilled radiologists and healthcare professionals is limited in many parts of the world. In low- and middle-income countries, the lack of trained medical personnel and diagnostic tools results in a high number of late-stage cancer diagnoses, which ultimately leads to poorer outcomes for patients.
AI’s ability to detect breast and ovarian cancers more accurately and efficiently offers hope for these underserved regions. By training AI models on large datasets of medical images, healthcare providers in remote areas can access the diagnostic power of AI without requiring a high level of specialized expertise. In these settings, AI can serve as a valuable adjunct to human clinicians, improving early detection rates and enabling better outcomes for patients.
In addition to improving detection accuracy, AI can help reduce healthcare costs associated with cancer diagnosis. By automating the interpretation of medical images, AI can speed up the diagnostic process, reduce the need for repeated tests, and ultimately lower the cost of healthcare delivery. This is particularly important in countries with limited healthcare resources, where cost-effective solutions are needed to address the growing burden of cancer.
The Challenges of Implementing AI in Clinical Practice
While the potential benefits of AI in cancer detection are clear, there are still several challenges to overcome before widespread implementation can occur. One of the primary concerns is the need for rigorous validation of AI models. In order for AI to be used in clinical practice, it must undergo extensive testing to ensure that it is safe, effective, and reliable. This includes ensuring that AI models can generalize across diverse populations and healthcare settings, as well as assessing their performance in real-world clinical environments.
Another challenge is the integration of AI into existing healthcare workflows. For AI to be truly effective in clinical practice, it must be seamlessly integrated into the diagnostic process. This requires collaboration between AI developers, healthcare professionals, and regulatory bodies to ensure that AI tools are user-friendly and can be easily incorporated into medical practices without disrupting patient care.
Data privacy and security are also critical concerns when using AI in healthcare. Medical data, including images, is highly sensitive, and ensuring that patient information is protected from unauthorized access is essential. As AI becomes more widespread in healthcare, it is important to establish robust data security protocols to safeguard patient privacy.
The Future of AI in Cancer Detection
Despite these challenges, the future of AI in cancer detection is incredibly promising. As AI continues to evolve, it is likely that we will see even more sophisticated models that can detect a broader range of cancers with even greater accuracy. AI has the potential to become an indispensable tool in the fight against cancer, helping to save lives through earlier and more accurate diagnoses.
The combination of AI’s efficiency, accuracy, and scalability makes it an ideal solution for addressing the global cancer burden. With further research, validation, and integration into healthcare systems, AI could play a pivotal role in revolutionizing cancer detection and improving outcomes for patients around the world.
The findings from studies in Germany and Sweden demonstrate the immense potential of AI in detecting breast and ovarian cancers. By leveraging the power of AI to analyze mammograms and ultrasound images, healthcare providers can improve the accuracy and efficiency of cancer detection, leading to earlier diagnoses and better patient outcomes. While challenges remain, the progress made so far suggests that AI will play a crucial role in the future of cancer screening and diagnosis, offering hope for healthier, longer lives for millions of people around the world.