San Francisco (California) [US], October 18: In the quest to unravel the mysteries of neurological diseases such as Alzheimer’s and multiple sclerosis, scientists may have discovered a game-changing factor. A study from the Gladstone Institutes reveals that leaked blood entering the brain through damaged blood vessels could be the key trigger behind several complex neurological disorders.
Unlike single-gene diseases like cystic fibrosis, most neurological diseases are far more complex. Even identical twins with the same genetic risk factors don’t always develop the same conditions. The reason? These disorders are influenced by a combination of environmental factors, genetic variants, and vascular risks such as high blood pressure and obesity.
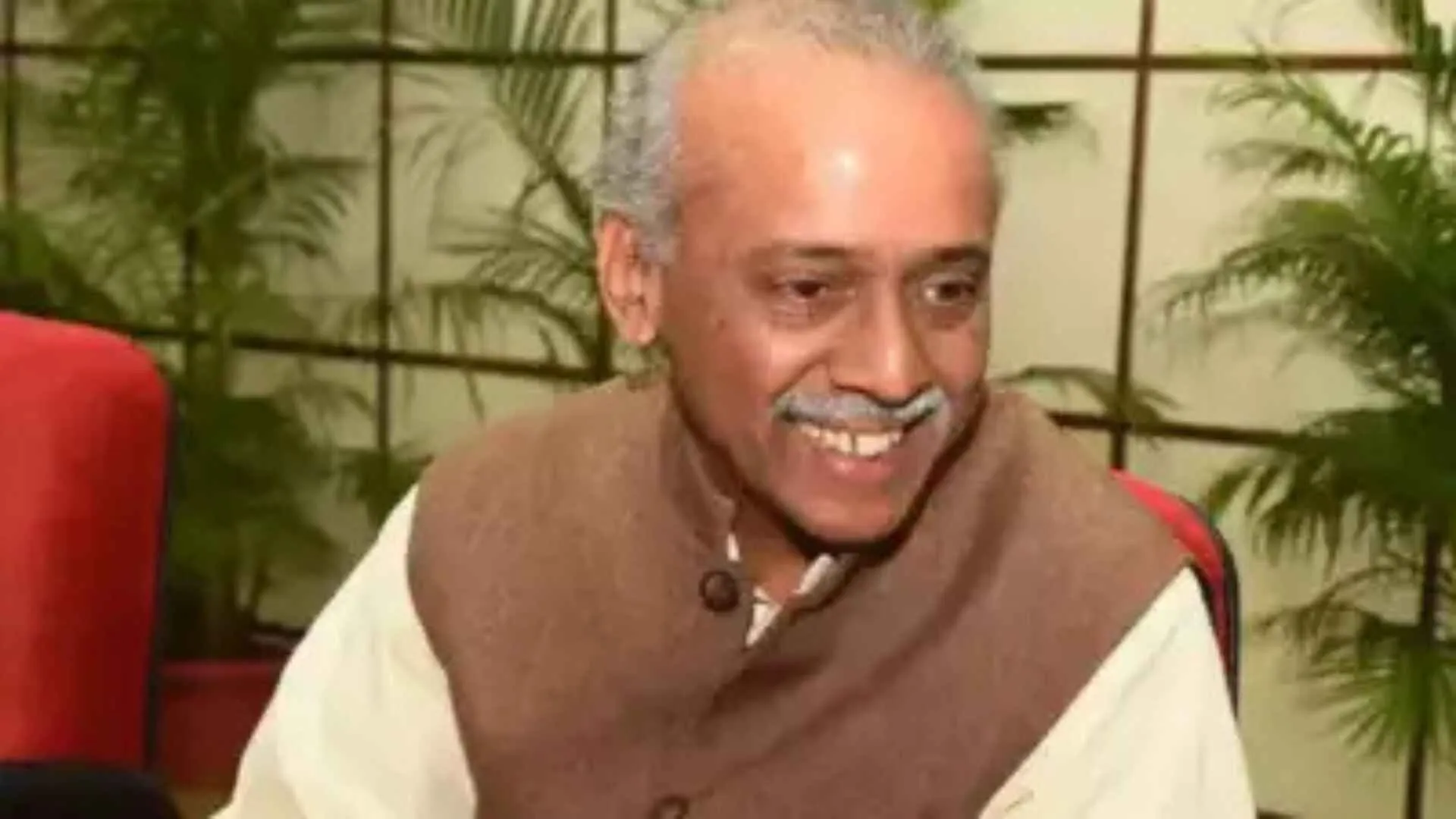
However, Katerina Akassoglou, PhD, a senior investigator at the Gladstone Institutes, believes there’s one hidden factor that unites these seemingly different diseases: toxic immune reactions caused by blood leaking into the brain.
Blood Leaks and Brain Inflammation: A Common Link in Neurological Diseases
“Interactions between the brain, blood vessels, and the immune system are a common thread in the progression of many neurological diseases that were traditionally viewed as unrelated,” says Akassoglou, who is also the director of the Center for Neurovascular Brain Immunology at Gladstone and UC San Francisco.
Her research, recently published in Cell as part of its 50th-anniversary “Focus on Neuroscience” issue, highlights how this leaked blood, particularly a protein called fibrin, triggers a harmful chain reaction. Normally involved in blood clotting, fibrin becomes toxic when it escapes the bloodstream and enters the brain, where it hijacks the brain’s immune system and causes irreversible damage to neurons.
This process has been found in a range of conditions—from Alzheimer’s and traumatic brain injuries to multiple sclerosis and even COVID-19-related brain damage.
Neutralizing the Culprit: A New Therapeutic Hope
The exciting part? Akassoglou’s team has developed a groundbreaking solution. By “neutralizing” fibrin’s toxic properties, they can halt the damaging process, providing protection against a host of neurological diseases—at least in animal models. The team has already developed a fibrin-targeting monoclonal antibody, a therapeutic drug that has shown promise in treating multiple sclerosis and Alzheimer’s in mice. Even more remarkable, this same approach has also been effective in addressing neurological complications from COVID-19.
Currently, a humanized version of this first-in-class fibrin immunotherapy is in Phase 1 clinical trials, offering a potential breakthrough for patients with complex neurological conditions.
A New Era of Treatment: The Blood-Brain-Immune Interface
Akassoglou and her colleagues argue that this novel understanding of the blood-brain-immune interface demands a shift in how we view neurological diseases. “We can no longer just focus on genes or environmental factors alone,” she says. “We need to look at the immune and vascular systems’ role in these diseases to discover better treatments.”
The next decade, they predict, will see major advances in treating neurological diseases through collaborative efforts that bring together neuroscientists, immunologists, hematologists, bioengineers, and drug developers. These interdisciplinary networks will spark innovation and drive the development of new drugs that target the immune system’s response to blood leaks in the brain.
A New Hope for Patients with Neurological Diseases
With this groundbreaking research, a new frontier in treating complex neurological diseases has opened. By targeting the blood-brain-immune interface, scientists are on the verge of unlocking treatments that could transform the lives of millions suffering from Alzheimer’s, multiple sclerosis, and beyond. As clinical trials progress, the future looks bright for these innovative therapies.