The devastating case of 22-year-old William Hewes, a history and politics student, has highlighted critical failures in hospital communication and medical protocols. An inquest into his death revealed that a delay in administering life-saving antibiotics at Homerton Hospital in east London contributed to his fatal deterioration from meningococcal septicaemia.
William’s mother, Dr. Deborah Burns, a consultant paediatrician at the same hospital, witnessed firsthand the series of medical missteps that led to his tragic passing. Despite her repeated warnings to doctors and nurses about the urgent need for antibiotics, a communication breakdown resulted in a crucial delay in his treatment. This article delves into what happened, the failures identified, and the implications for medical practice.
The Timeline of Events Leading to William’s Death
William’s Deteriorating Condition
On January 21, 2023, just after midnight, Dr. Deborah Burns rushed her son to Homerton Hospital’s A&E department. Recognizing the severity of his symptoms, she immediately informed medical staff that he might have meningitis and required urgent treatment.
A doctor quickly prescribed 2 grams of ceftriaxone, an antibiotic essential for treating meningococcal infections. However, due to a communication mix-up, the medication was not administered within the critical first hour.
The Critical Delay in Administering Antibiotics
Dr. Burns repeatedly voiced her concerns, warning that her son had not yet received the prescribed antibiotics. Despite assurances that the drug had been “written up,” it was not actually given.
Dr. Luke Lake, the acting medical registrar, later admitted that he failed to ensure the drug was administered promptly. While he claimed to have checked William’s chart earlier, he could not confirm whether he independently realized the mistake or if it was Dr. Burns’s prompting that made him investigate.
By the time the oversight was addressed, vital time had been lost, and William’s condition had worsened.
Breakdown in Medical Communication and Oversight
Doctor and Nurse Miscommunication
The inquest revealed that Dr. Rebecca McMillan, the duty emergency registrar, assumed that her instructions to administer ceftriaxone were clear. However, nurse Marianela Balatico later admitted that the instruction “slipped my mind” as she focused on treating William’s symptoms instead.
Dr. McMillan recounted her distress upon realizing the medication had not been administered. “I obviously thought my instructions were clear enough,” she told the court. She later acknowledged that one of the key learning points from this tragedy was the need for explicit clarity in delegating tasks to medical staff.
Disagreements Over Intensive Care Admission
The inquest also heard how doctors debated whether William should be admitted to the intensive care unit (ICU) sooner.
Dr. McMillan pleaded with Dr. Mathuratha Sivasubramanian, the intensive care registrar, to transfer William to ICU as his symptoms worsened. However, Dr. Sivasubramanian insisted on continuing treatment in the emergency unit before reassessing his condition.
The coroner, Mary Hassell, described the exchange as an argument, to which Dr. McMillan responded: “She [Dr. Sivasubramanian] wasn’t behaving with the same urgency that I was conveying.”
This disagreement further delayed critical intervention, leaving William in a deteriorating state without the intensive support he needed.
Sepsis and Meningococcal Septicaemia: The Deadly Race Against Time
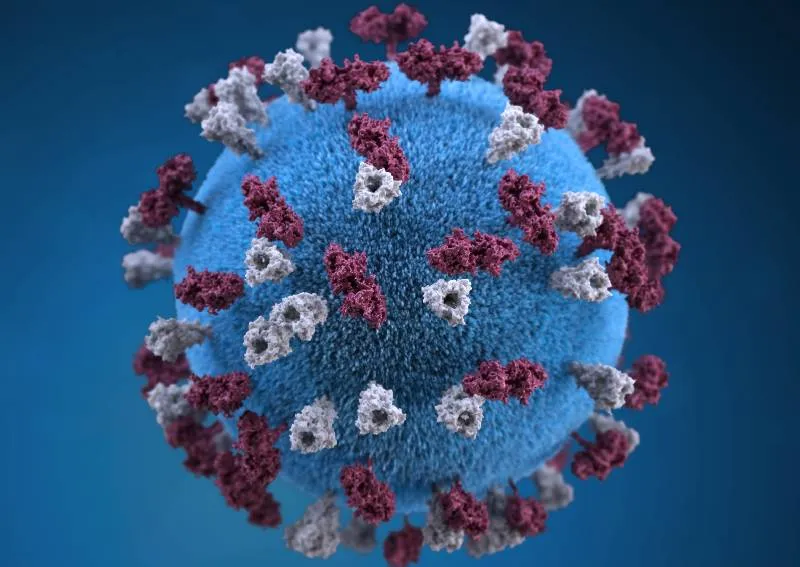
Sepsis is a life-threatening condition triggered by the body’s extreme response to an infection. Meningococcal septicaemia, caused by the Neisseria meningitidis bacterium, spreads rapidly through the bloodstream, causing organ failure and death if not treated immediately.
Why Timing is Crucial in Sepsis Cases:
- The “golden hour” is the first 60 minutes of treatment, where administering antibiotics can significantly improve survival rates.
- A delay of even one hour in sepsis cases can increase the risk of death by up to 8%.
- Meningococcal infections can progress within hours, making rapid antibiotic administration and ICU support essential.
In William’s case, the delay in receiving antibiotics allowed the infection to spread unchecked, leading to irreversible organ damage.
Key Failures Identified in the Inquest
-
Lack of Clear Communication:
- Medical staff assumed antibiotics had been given but failed to confirm or follow up.
- Instructions to administer medication were not properly recorded or checked.
-
Breakdown in Accountability:
- The responsibility for William’s care was unclear, with multiple doctors assuming others were in charge.
- Dr. McMillan later admitted she did not know who had ultimate oversight of William’s treatment.
-
Failure to Recognize Urgency:
- Despite clear symptoms of sepsis, ICU admission was debated instead of being expedited.
- The delay in transferring William meant he did not receive the intensive care he needed in time.
The Aftermath: Calls for Change in Medical Protocols
The heartbreaking loss of William Hewes has led to renewed calls for better communication and accountability in emergency care.
Lessons from the Inquest:
- Mandatory Double-Checking: All life-saving drug orders should be verified by multiple staff members to prevent oversight.
- Real-Time Digital Tracking: Hospitals should use real-time tracking systems to ensure prescribed drugs are administered without delay.
- Clear Role Assignments: Every patient should have a designated lead doctor responsible for overseeing their care from admission to treatment.
- Stronger Training in Sepsis Response: Medical professionals must be trained to recognize sepsis early and act without delay.
Dr. Burns, in her emotional testimony, emphasized that no other family should suffer the same devastating loss due to medical negligence.
A Preventable Tragedy
William Hewes’s death was a tragic reminder of how small errors in communication can have fatal consequences. A simple confirmation of whether antibiotics were given could have saved his life. The inquest highlighted critical gaps in hospital procedures that must be addressed to prevent similar tragedies in the future.
While nothing can bring William back, his story serves as a wake-up call for the urgent need to improve emergency medical protocols, enhance accountability, and ensure that life-saving treatments are never delayed again.