In a groundbreaking development, scientists are working on a new injectable contraceptive system that creates a long-lasting implant within the body. This innovative method, which is still in its early stages, could revolutionize not only birth control but also the delivery of a wide range of drugs over extended periods of time. The approach could help address critical challenges in both the medical and healthcare fields, particularly in areas with limited access to healthcare services.
The Current Landscape of Contraceptive Options
Contraceptive implants are a popular method of birth control, offering long-term protection without the need for daily intervention. These devices, which are inserted by healthcare professionals, can remain effective for several years. However, while they offer convenience, they come with the downside of requiring a small surgical procedure for insertion, which may not be feasible or desirable for all women.
On the other hand, contraceptive injections are another well-established form of birth control. These injections offer convenience over pills, as they do not require daily administration. However, the major limitation of these injections is their short duration of effectiveness—typically, they only last for three months. This has led to the search for more long-term solutions that do not involve invasive procedures and that can be managed with minimal medical intervention.
The New Approach: Self-Assembling Contraceptive Implants
Now, researchers have taken a significant step forward in contraceptive technology with the development of a self-assembling long-acting contraceptive implant. While the concept of such implants is not entirely new, the method being proposed here is unique in that it eliminates the need for a medical professional to perform an invasive procedure. Instead, the implant is created inside the body through an injection that can be administered easily with a small needle.
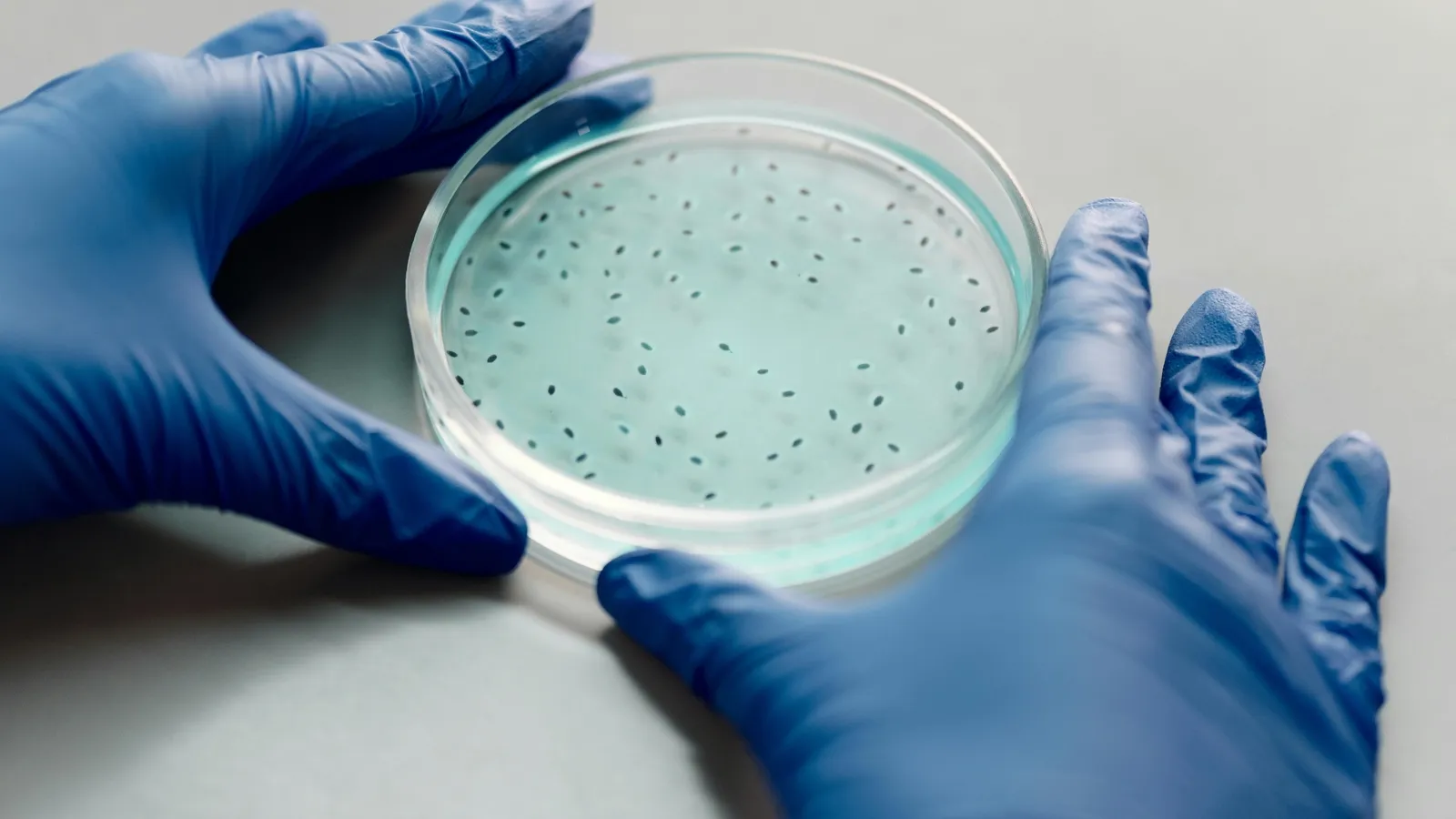
The process involves injecting micro-crystals of a synthetic version of the hormone progesterone into the body. These micro-crystals are suspended in a solvent that does not mix well with water. Once injected, the solvent begins to exchange with the fluids in the body. As the solvent interacts with bodily fluids, the micro-crystals tend to clump together, forming larger crystals. Over time, these crystals solidify, creating a solid implant inside the body. This implant slowly releases the hormone progesterone over an extended period, providing long-lasting contraceptive effects.
A Broader Application for Drug Delivery
While the focus of the research has been on developing a contraceptive implant, the scientists involved in the study are excited about the broader potential of this technology. Dr. Giovanni Traverso, a co-author of the study and a gastroenterologist at Brigham and Women’s Hospital in the United States, explained that this technology could have applications beyond birth control. The approach could be used for delivering other drugs that are poorly soluble in water but require long-term delivery. These include treatments for conditions such as HIV, tuberculosis (TB), schizophrenia, chronic pain, and metabolic diseases.
One of the key advantages of this method is that it could provide a simple and cost-effective solution for delivering medications in low-resource settings, where access to healthcare and ongoing medical supervision is often limited. The ability to inject a drug that forms its own implant inside the body would mean that patients would not have to visit healthcare facilities regularly to receive their medications. This could be especially beneficial for patients who struggle with medication adherence or who live in remote areas.
Promising Results from Animal Studies
The team of researchers behind this innovation has successfully completed proof-of-concept experiments in rats, allowing them to refine the choice of solvent in the injection. The results of these experiments have been promising. In the rats, the micro-crystals formed a solid implant, and the release of the progesterone hormone was sustained for at least 97 days. Dr. Traverso noted that there is potential for longer durations of drug release, depending on adjustments to the formulation. The flexibility of the technology could allow for multi-year dosing, which would be a significant improvement over current contraceptive options that require regular injections.
One of the most attractive aspects of this self-assembling implant is its reversibility. If necessary, the implant can be removed, offering flexibility for patients who may wish to discontinue its use. Furthermore, the injection method is compatible with small needles, making it relatively painless and non-invasive compared to other long-acting contraceptive methods.
Challenges and Future Prospects
Despite the promising early results, this research is still in its early stages, and the efficacy and safety of the approach have yet to be tested in humans. The team is currently focused on refining the technology and conducting additional studies to determine how it can be scaled up for human use. Dr. Traverso emphasized that the next few years will be crucial for validating the technology and ensuring that it is both safe and effective for human patients.
“The groundwork for future human studies is laid, and we hope to begin clinical trials in the next three to five years,” said Dr. Traverso. These trials will be essential to determine how well the implant works in real-world settings and whether it can be used as a reliable and safe alternative to current contraceptive methods.
Expert Opinions and Support
Dr. Janet Barter, the president of the Faculty of Sexual and Reproductive Healthcare, expressed her excitement about the potential of this new technology. She believes that the self-assembling implant could provide a convenient and innovative option for individuals in low-resource settings, where access to regular healthcare services is often limited. She further stated that this innovation could be an essential tool for individuals who have difficulty accessing or affording traditional forms of contraception.
However, Dr. Barter also emphasized the need for further research into the safety, efficacy, and accessibility of this technology. She encouraged the researchers to work closely with potential users to ensure that the implant meets the needs and preferences of those who would rely on it. She acknowledged that while the approach shows great promise, careful attention must be paid to the diverse needs of different populations and healthcare systems.
The Potential Impact on Global Health
If the self-assembling contraceptive implant proves successful in human trials, it could significantly impact global health, particularly in regions where access to contraception is limited. In many parts of the world, women face challenges in obtaining reliable birth control due to financial, cultural, or logistical barriers. A self-administered, long-acting contraceptive implant could give women greater autonomy over their reproductive health, allowing them to manage family planning without relying on frequent visits to healthcare providers.
Additionally, the broader applications of this technology could transform the treatment landscape for many chronic diseases. For example, in resource-limited settings, long-acting drug delivery systems could enable the treatment of HIV, TB, and other diseases without the need for regular medical visits. This could help improve patient outcomes by ensuring consistent medication adherence and reducing the burden on healthcare systems.
The development of a self-assembling contraceptive implant represents a major step forward in the field of long-acting drug delivery. While the technology is still in its early stages, the potential benefits are vast, not only for birth control but also for the treatment of a wide range of chronic conditions. If successful, this approach could offer a simple, non-invasive, and cost-effective way to administer medication over extended periods, benefiting individuals in low-resource settings and improving global health outcomes. With further research and development, this breakthrough could pave the way for a new era of drug delivery, offering hope for millions of people worldwide.