Researchers Find Vital Link Between Inflammation and Depression
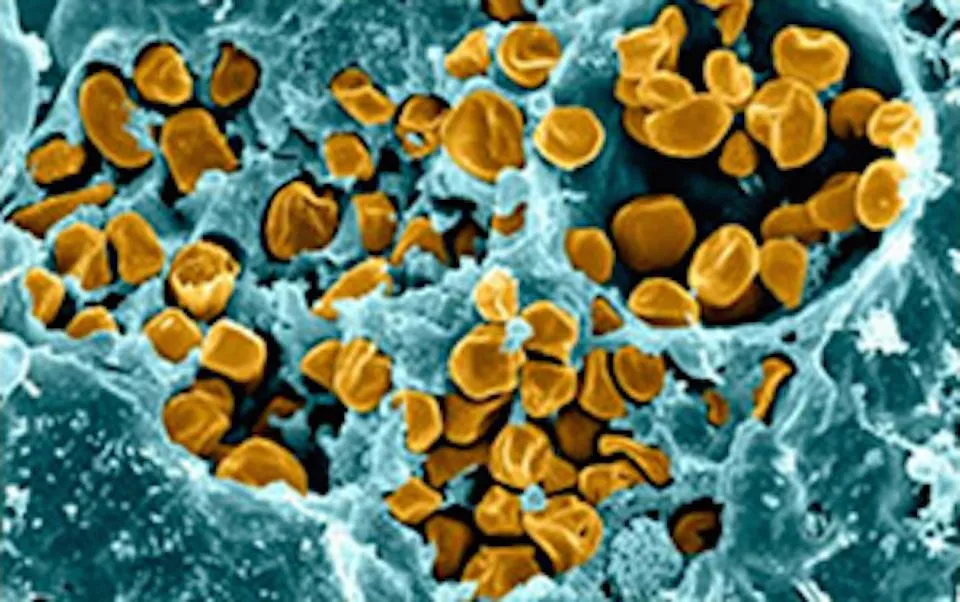
Depression is often perceived as a purely psychological condition, but recent research has revealed that its roots may extend far beyond the brain. A groundbreaking study has found a crucial link between inflammation in the body and the onset of depression. This discovery is reshaping how mental health professionals approach diagnosis, treatment, and prevention of depressive disorders.
Inflammation, a biological process meant to protect the body from infections and injuries, can become harmful when it turns chronic. Researchers are now uncovering how this persistent state of inflammation might influence the brain and mental health, offering new hope for those struggling with depression.
This article explores the relationship between inflammation and depression, the scientific evidence supporting this link, and what it means for the future of mental health treatment.
1. What Is Inflammation?
Inflammation is the body’s natural response to threats like infections, injuries, or toxins. It is designed to help the body heal and protect itself.
- Acute Inflammation: A short-term response that helps repair damaged tissues.
- Chronic Inflammation: A prolonged state of inflammation that can damage healthy tissues and lead to various health issues, including cardiovascular diseases, diabetes, and now, depression.
Chronic inflammation often results from factors like poor diet, stress, sedentary lifestyle, and autoimmune conditions.
2. Understanding Depression: Beyond the Brain
Depression affects millions of people globally, characterized by persistent sadness, loss of interest in activities, and difficulty functioning in daily life. While depression has long been linked to chemical imbalances in the brain, researchers now suggest it is a multifaceted condition involving:
- Neurotransmitters: Such as serotonin and dopamine.
- Genetic Predisposition: A family history of depression increases risk.
- External Factors: Stress, trauma, and environmental influences.
- Biological Mechanisms: Including inflammation.
This new understanding underscores the importance of looking beyond the brain to identify the underlying causes of depression.
3. The Inflammation-Depression Connection
Recent studies suggest that inflammation plays a significant role in depression. Chronic inflammation can affect the brain by:
- Producing Pro-Inflammatory Cytokines: These proteins, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), can interfere with brain function and mood regulation.
- Disrupting Neurotransmitters: Inflammation can reduce the production of serotonin, a key neurotransmitter involved in mood regulation.
- Affecting Neuroplasticity: Chronic inflammation may hinder the brain’s ability to form new neural connections, essential for learning and emotional resilience.
Research indicates that individuals with elevated inflammatory markers are more likely to experience depression.
4. Key Scientific Studies
Several studies have provided compelling evidence for the link between inflammation and depression:
1. The Cytokine Hypothesis of Depression
This theory suggests that elevated levels of pro-inflammatory cytokines can induce depressive symptoms by affecting brain function.
2. The Role of C-Reactive Protein (CRP)
CRP is a marker of inflammation in the body. Studies have shown that individuals with higher CRP levels are more likely to report symptoms of depression.
3. Inflammatory Diseases and Depression
Conditions like rheumatoid arthritis, characterized by chronic inflammation, have higher rates of depression, further supporting the connection.
4. Antidepressants and Inflammation
Some antidepressants have been found to reduce inflammatory markers, indicating that part of their effectiveness may lie in their anti-inflammatory properties.
5. Inflammation and Stress
Stress is a known trigger for both depression and inflammation. When the body is exposed to chronic stress, it releases cortisol, the stress hormone, which can:
- Increase inflammation by altering immune system function.
- Damage the hippocampus, a brain region critical for mood regulation and memory.
This vicious cycle of stress, inflammation, and depression creates a complex interplay that requires a multifaceted treatment approach.
6. Lifestyle Factors Contributing to Chronic Inflammation
Chronic inflammation is influenced by several lifestyle factors, many of which are also linked to depression:
1. Poor Diet
- High consumption of processed foods, sugar, and trans fats can promote inflammation.
- Deficiencies in omega-3 fatty acids, vitamins, and minerals may exacerbate both inflammation and depression.
2. Lack of Exercise
- Physical inactivity contributes to inflammation and can lead to poor mental health.
3. Poor Sleep
- Sleep deprivation increases inflammatory markers and impairs emotional regulation.
4. Substance Abuse
- Excessive alcohol and drug use can promote inflammation and increase the risk of depression.
5. Chronic Stress
- Psychological stress is a potent driver of inflammation and mental health challenges.
7. Implications for Treatment
The link between inflammation and depression is transforming how mental health conditions are treated. Some promising approaches include:
1. Anti-Inflammatory Medications
- Non-steroidal anti-inflammatory drugs (NSAIDs) and cytokine inhibitors are being explored as potential treatments for depression.
2. Nutritional Interventions
- Anti-inflammatory diets rich in fruits, vegetables, whole grains, and omega-3 fatty acids can reduce inflammation and improve mood.
- Probiotics and gut health play a role in reducing inflammation and supporting mental health.
3. Physical Activity
- Regular exercise reduces inflammation, improves mood, and enhances overall well-being.
4. Stress Management
- Mindfulness, meditation, and yoga are effective in reducing stress and inflammation.
5. Personalized Medicine
- Biomarkers for inflammation may help identify individuals who could benefit from targeted anti-inflammatory treatments for depression.
8. The Role of the Gut-Brain Axis
The gut-brain axis, a bidirectional communication system between the gut and the brain, is also implicated in the inflammation-depression link.
- Gut Microbiota: Imbalances in gut bacteria can lead to increased inflammation and depressive symptoms.
- Dietary Interventions: A healthy gut microbiome, supported by probiotics and prebiotics, can help reduce inflammation and improve mental health.
This emerging area of research highlights the interconnectedness of physical and mental health.
9. Breaking the Stigma
The discovery of the inflammation-depression link challenges the stigma surrounding mental health conditions.
- Depression is not just a “weakness” or “chemical imbalance” but a complex interplay of biological, psychological, and environmental factors.
- Recognizing the physical underpinnings of depression can help reduce stigma and encourage individuals to seek treatment.
10. Future Directions
As research progresses, new avenues for understanding and treating depression are emerging:
- Biomarker Identification: Identifying specific inflammatory markers for tailored treatment plans.
- Combination Therapies: Integrating anti-inflammatory treatments with traditional antidepressants for better outcomes.
- Preventive Measures: Promoting anti-inflammatory lifestyles to prevent depression before it starts.
The integration of mental health and physical health research is paving the way for more holistic approaches to healthcare.
The vital link between inflammation and depression is a game-changer in the field of mental health. By addressing the biological roots of depression, researchers and healthcare professionals can offer more effective, personalized treatments to those in need.
This discovery underscores the importance of a holistic approach to mental health—one that considers the interconnectedness of the mind and body. With continued research, innovative treatments, and public awareness, the future holds promise for millions of individuals battling depression.