Candida auris, commonly known as C. auris, has emerged as a significant and dangerous health threat in the United States, especially in hospitals and nursing homes. This highly drug-resistant fungus has become a cause for concern, as it continues to spread rapidly and silently across healthcare settings, making it difficult for medical professionals to contain and treat. In 2023, the Centers for Disease Control and Prevention (CDC) issued a stern warning regarding the rising cases of C. auris, emphasizing its deadly potential and rapid spread.
What is Candida Auris (C. Auris)?
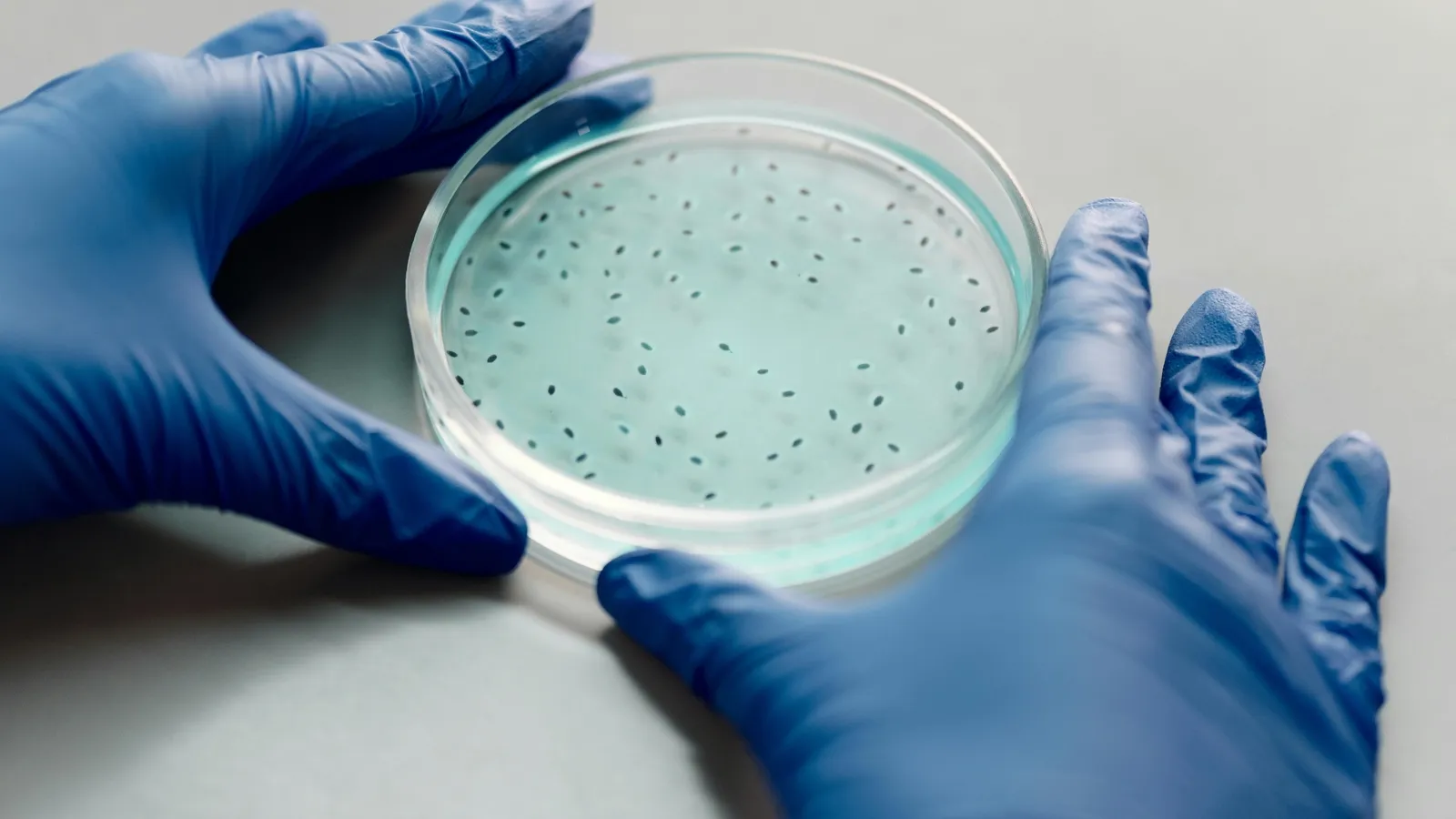
Candida auris is a type of yeast that can cause severe infections in humans, particularly in healthcare environments. It was first identified in Japan in 2009, but it wasn’t until 2016 that it made its presence known in the United States. Since then, the infection rate has increased exponentially, with C. auris now posing a serious threat to hospital patients, particularly those with weakened immune systems or other pre-existing conditions. The fungus can be transmitted through contaminated surfaces or medical equipment, often thriving in the humid and sterile environments found in hospitals and nursing homes.
One of the most concerning aspects of C. auris is its ability to resist multiple antifungal treatments, making infections difficult or sometimes impossible to treat. This antifungal resistance has earned it a place in the CDC’s list of “urgent antimicrobial resistance threats,” which calls for heightened awareness, more research, and rapid response strategies.
The Rapid Spread and Escalating Cases
In 2016, the U.S. saw a relatively low number of C. auris infections—only 52 cases across the country. However, by 2023, the situation had escalated dramatically, with 4,514 confirmed cases. This dramatic rise in infections is a clear indication of how fast the fungus is spreading. The CDC attributes this increase to various factors, including the fungus’s ability to persist on surfaces, its resistance to typical disinfectants, and the lack of awareness in healthcare facilities. As of now, C. auris has been reported in at least 27 U.S. states, with the most severe outbreaks occurring in large hospitals and nursing homes.
The growing number of cases has prompted healthcare officials to call for urgent improvements in infection control practices, including better sanitation procedures, faster diagnostic tools, and more effective treatments.
How Dangerous is C. Auris?
C. auris can cause a wide range of infections, from superficial skin conditions to life-threatening bloodstream infections. It primarily affects immunocompromised individuals, such as those with weakened immune systems, diabetes, or underlying heart and lung diseases. C. auris infections are often resistant to common antifungal medications, meaning that standard treatments may not work, and doctors must turn to more powerful and expensive drugs that may still offer limited success.
The mortality rate associated with C. auris is concerning. The CDC estimates that between 30% and 60% of patients with C. auris infections have died, though it’s important to note that many of these patients had additional severe health conditions that contributed to their death. Nevertheless, the fact that this fungus is responsible for so many fatalities underlines the urgent need for better management and prevention strategies.
Epidemiologists are particularly concerned about the rise of C. auris due to its ability to spread so rapidly in hospital settings, where vulnerable patients are at an increased risk of infection. Furthermore, C. auris is capable of surviving on hospital surfaces for extended periods, making it difficult to eliminate through standard cleaning protocols. This resistance to cleaning and disinfection methods allows the fungus to persist in healthcare environments, potentially infecting new patients.
CDC Response and Growing Concern
In 2023, the CDC issued a formal warning about C. auris, highlighting its growing spread in hospitals, nursing homes, and long-term care facilities. The agency emphasized the need for comprehensive infection prevention measures, including more widespread use of surveillance, laboratory testing, and prompt action to contain outbreaks.
The CDC also called for expanded laboratory capacity, which would allow healthcare providers to detect C. auris infections more quickly and respond accordingly. Early detection is crucial, as delayed diagnoses can lead to worsened patient outcomes, particularly for those already suffering from other conditions. The CDC stressed that healthcare providers must adhere to infection control protocols, such as regular cleaning and disinfecting of medical equipment and surfaces, to minimize the risk of transmission.
Dr. Meghan Lyman, an epidemiologist at the CDC, noted, “The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control.” These strategies are seen as essential to curbing the spread of C. auris and preventing further public health risks.
Challenges in Treatment and Diagnosis
One of the most significant challenges in addressing C. auris infections is the lack of effective treatment options. The fungus has developed resistance to multiple classes of antifungal drugs, making it more difficult to treat once it enters a patient’s system. Current treatment options are limited and often ineffective, forcing medical professionals to rely on more aggressive approaches that come with higher costs and more potential side effects.
In addition to treatment challenges, diagnosing C. auris infections is difficult. The fungus is not always detected by traditional laboratory methods, which can lead to delayed diagnoses and improper treatment. Researchers are working to develop faster and more accurate diagnostic tests, but for now, healthcare providers are left with limited resources to identify the fungus in a timely manner.
Impact on Healthcare Settings
Infected patients typically require extended hospital stays, which can increase the strain on already overburdened healthcare systems. The fungus has a high transmission rate, which means that it can spread rapidly in crowded healthcare settings. Patients who are already critically ill or undergoing surgery are particularly vulnerable to C. auris infections.
The growing prevalence of C. auris in healthcare settings also raises concerns about the adequacy of hospital hygiene standards. Regular cleaning of patient rooms, medical equipment, and surfaces is essential to prevent the spread of infections, but C. auris is particularly resilient to disinfectants, making it more difficult to eliminate from hospital environments.
Hospitals are being forced to adopt additional infection control measures to combat C. auris, which may include isolating affected patients, implementing stricter sanitation procedures, and limiting access to certain areas of the facility. These measures are necessary to reduce the risk of transmission, but they come with challenges related to cost, resources, and staffing.
Prevention and Control Measures
Given the rapid spread and high mortality rate associated with C. auris, it is crucial to implement effective infection control strategies in hospitals and nursing homes. Healthcare professionals must adhere to rigorous hygiene protocols, including frequent handwashing, disinfection of medical equipment, and isolation of infected patients to prevent cross-contamination.
In addition to hospital-level precautions, public health authorities are calling for increased awareness of C. auris among healthcare providers. Regular training on recognizing the symptoms and transmission routes of the fungus is essential for preventing outbreaks. Hospitals must also ensure that they have the necessary resources to conduct routine screening and testing for C. auris infections, particularly in high-risk areas like intensive care units and surgical wards.
Healthcare institutions are also being urged to improve their surveillance systems to detect C. auris cases early and prevent outbreaks from spiraling out of control. Rapid detection and prompt isolation are key to containing the spread of the fungus.
The ongoing spread of C. auris highlights the growing threat posed by antimicrobial-resistant pathogens in healthcare settings. While research into new antifungal treatments and diagnostic tools is ongoing, C. auris serves as a stark reminder of the need for continued investment in infection prevention and control measures.
Public health authorities, researchers, and healthcare providers must work together to address the challenges posed by C. auris and other antimicrobial-resistant infections. Given its ability to spread quickly and resist treatment, C. auris represents a serious public health concern that requires swift action to protect vulnerable patients and prevent further outbreaks.
In conclusion, C. auris is a deadly and highly resistant fungus that is rapidly spreading across the United States, posing significant challenges for healthcare systems. Its resistance to multiple antifungal drugs and its ability to persist in healthcare environments make it a particularly dangerous pathogen. Efforts to control its spread through better infection prevention, improved diagnostics, and stronger surveillance systems are critical to combating this growing public health threat.