Social Program Cuts Tuberculosis Cases Among Brazil’s Poorest by More Than Half
In recent years, Brazil has made remarkable strides in reducing the burden of tuberculosis (TB) within its most vulnerable populations. A groundbreaking social program, aimed at tackling the root causes of the disease, has led to a more than 50% decrease in TB cases among Brazil’s poorest communities. This achievement reflects the intersection of health policy, socioeconomic support, and community-based interventions, highlighting the critical role of addressing both medical and social determinants of health.
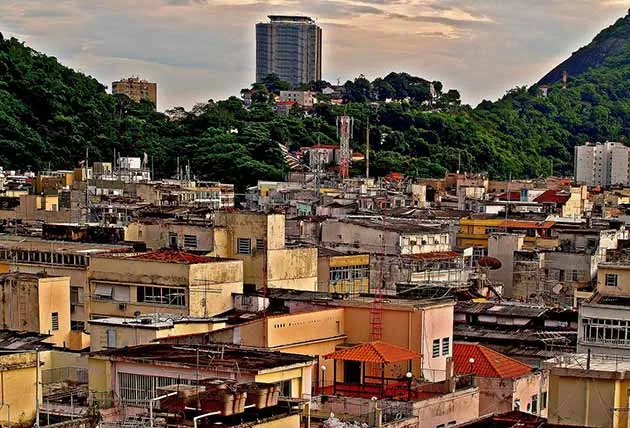
Tuberculosis remains one of the world’s deadliest infectious diseases, with millions of new cases reported annually. In Brazil, the country’s poorest regions have historically borne the brunt of the disease, where poverty, overcrowded living conditions, inadequate healthcare access, and poor nutrition have created an ideal environment for the spread of TB. However, through comprehensive and well-targeted social programs, Brazil has seen a significant decline in cases, particularly among the poorest groups, offering an innovative model for addressing public health crises in resource-limited settings.
Tuberculosis in Brazil: A Persistent Public Health Challenge
Tuberculosis (TB) is caused by the bacterium Mycobacterium tuberculosis and primarily affects the lungs. Although it is a curable disease, TB remains one of the leading causes of death from infectious diseases worldwide. In Brazil, despite efforts to combat TB through national programs such as the National Tuberculosis Control Program (PNCT), the disease has remained a major public health issue, particularly in impoverished urban and rural areas.
Brazil’s socioeconomic disparity has contributed significantly to the country’s TB burden. In the poorest areas, particularly in favelas (slums) and indigenous territories, overcrowding, poor sanitation, lack of access to medical services, and malnutrition exacerbate the spread of TB. These regions are often characterized by limited healthcare infrastructure, a shortage of healthcare workers, and difficulties in reaching marginalized communities with effective preventive and treatment interventions.
In 2020, Brazil ranked 16th globally for the highest number of new TB cases. The disease predominantly affects adults aged 15-49, and the poorest populations are particularly vulnerable due to their heightened exposure to risk factors such as poor living conditions, smoking, and HIV co-infection. TB, along with its associated comorbidities, presents a significant challenge for Brazil’s public health system.
The Role of Social Determinants in Tuberculosis Spread
While TB is primarily an infectious disease, its spread and impact are deeply influenced by the social determinants of health. These factors include economic stability, education, social and community networks, and living conditions. In Brazil’s poorest regions, these determinants interact in complex ways to increase the risk of TB transmission and worsen its outcomes.
- Overcrowding: Overcrowded living conditions in informal settlements and slums increase the likelihood of TB transmission. Poor ventilation and inadequate housing make it difficult to prevent the spread of airborne infections like TB.
- Poor Nutrition: Malnutrition, often seen in low-income populations, weakens the immune system, making individuals more susceptible to infection. Proper nutrition is critical for building immunity and supporting the body’s ability to fight off diseases like TB.
- Limited Access to Healthcare: In many of Brazil’s poorest regions, access to healthcare services is limited, with long wait times, lack of transportation, and financial barriers to seeking care. This results in delayed diagnoses and treatment, increasing the risk of disease progression and transmission.
- HIV Co-infection: HIV is a known risk factor for TB, as it weakens the immune system and makes it harder for the body to fight off TB bacteria. The prevalence of HIV in impoverished areas exacerbates the TB burden.
- Stigma and Social Marginalization: TB is often stigmatized in communities, leading individuals to delay seeking treatment for fear of discrimination. Social isolation and a lack of support networks can also hinder adherence to TB treatment regimens.
The Social Program That Transformed TB Outcomes
In response to these challenges, Brazil launched a comprehensive social program designed to address the root causes of TB within its most vulnerable populations. The program, which integrates healthcare access, social services, and community support, has proven to be a pivotal factor in the significant reduction of TB cases in impoverished areas.
The program’s core components include:
1. Improved Access to Healthcare and Early Diagnosis
One of the most important elements of the program is improving access to healthcare services for Brazil’s poorest populations. The program has focused on ensuring that individuals in marginalized communities have easier access to diagnostic testing and treatment for TB. This includes:
- Mobile clinics: Mobile healthcare units were deployed to provide services in underserved areas, ensuring that individuals who could not access traditional healthcare facilities received care.
- Community health workers: Trained community health workers have been stationed in vulnerable communities to offer education, counseling, and support for individuals at risk of TB. These workers also help to identify symptoms of TB early and facilitate timely referrals for testing and treatment.
- Increased availability of diagnostic tests: The introduction of more accessible and affordable TB diagnostic tests, including rapid molecular tests and chest X-rays, has made it easier for healthcare providers to diagnose TB early and begin treatment promptly.
2. Social Support and Economic Assistance
Recognizing that poverty is a major barrier to TB prevention and treatment, the program also addresses the social and economic needs of vulnerable populations. Key strategies include:
- Cash transfers: Direct cash transfers are provided to families affected by TB, helping them meet basic needs such as food, housing, and transportation to healthcare facilities.
- Nutritional support: Nutritional interventions, including the provision of food aid and access to nutrition programs, aim to improve the immune systems of individuals at risk and those undergoing TB treatment.
- Subsidized medications: To ensure that all individuals can access the medications they need, the program has made TB medications available free of charge, removing financial barriers to treatment.
3. Public Health Education and Community Engagement
Raising awareness about TB, its symptoms, and the importance of early treatment has been a critical component of the program. Public health campaigns have focused on:
- Community-based education: Local leaders and healthcare workers educate the public about TB prevention and treatment, as well as the importance of completing the full course of medication to prevent resistance.
- Reducing stigma: Efforts have been made to reduce the stigma surrounding TB by promoting understanding and encouraging community support for individuals undergoing treatment.
- Collaboration with community organizations: The program has partnered with local organizations to provide emotional and social support for individuals affected by TB, helping to improve treatment adherence and quality of life.
4. Addressing Co-morbidities and Risk Factors
The social program also addresses co-morbidities that exacerbate the TB burden, particularly HIV. People living with HIV are at a higher risk of developing TB, and the program integrates TB and HIV services to ensure that individuals with both conditions receive comprehensive care. This includes:
- Integrated testing and treatment: Co-infected individuals are tested and treated for both TB and HIV simultaneously, improving health outcomes and preventing further spread of the diseases.
- Antiretroviral therapy: The program ensures that people living with HIV have access to antiretroviral therapy, which strengthens the immune system and reduces the likelihood of developing TB.
Impact of the Social Program
The social program has proven to be highly successful, leading to a dramatic reduction in TB cases among Brazil’s poorest populations. Some of the key outcomes include:
- Over 50% reduction in TB cases: As a result of the program, TB incidence in the poorest communities has dropped by more than half. This is a remarkable achievement, considering the historical challenges posed by poverty, inadequate healthcare access, and other social determinants.
- Increased treatment adherence: The program’s combination of healthcare access, social support, and education has led to improved treatment adherence rates, reducing the likelihood of drug-resistant TB and ensuring that individuals complete their treatment regimens.
- Improved quality of life: The provision of social support, nutritional assistance, and financial aid has improved the overall quality of life for individuals affected by TB, helping them to better manage their condition and avoid social isolation.
- Strengthened public health infrastructure: The success of the program has also strengthened Brazil’s overall public health infrastructure, enhancing the country’s ability to respond to future outbreaks of TB and other infectious diseases.
Broader Implications for Global TB Control
The success of Brazil’s social program has significant implications for global TB control. The program provides a model for other countries, particularly those with high TB burdens and large impoverished populations. By addressing the social determinants of health, rather than just focusing on medical treatment alone, the program has demonstrated that a comprehensive, multi-faceted approach can effectively reduce TB transmission and improve health outcomes.
Moreover, the integration of social services, healthcare, and education is a model that could be applied to other infectious diseases, particularly in low-resource settings. The lessons learned from Brazil’s success in combating TB among its poorest populations could inform future public health interventions worldwide.
Brazil’s social program, which integrates healthcare, social services, and community support, has proven to be a powerful tool in reducing TB cases among the country’s poorest populations. By addressing both the medical and social determinants of health, the program has significantly decreased TB incidence, improved treatment adherence, and strengthened public health infrastructure. The success of this program offers valuable lessons for other countries facing similar challenges in the fight against tuberculosis and provides hope for the global effort to eliminate this deadly disease.