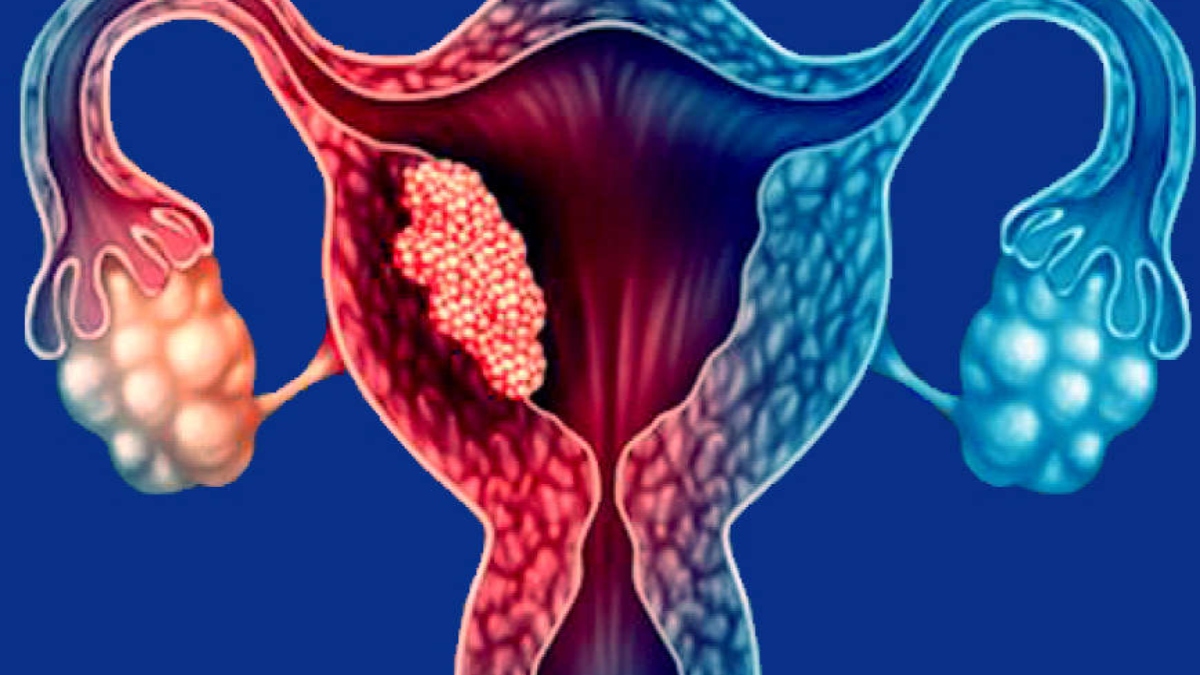
Endometrial cancer is the most common type of uterine cancer that begins in the inner lining of the uterus – the endometrium. Endometrial cancer occurs when the cells of the endometrium start multiplying rapidly and abnormally. This may thicken the lining of the uterus in certain places forming a mass of tissue i.e., a tumour. Endometrial cancer is often detected early as it frequently causes abnormal vaginal bleeding.
Risk factors:
The risk of endometrial cancer increases with hormonal imbalances i.e., the increase in the oestrogen (women’s hormone) levels leading to changes in the endometrium. Women who undergo early menstruation or late menopause, have excess body fat, diabetes or have a genetic predisposition to cancer or take estrogen-only hormone replacement therapy after menopause or take tamoxifen to prevent or treat breast cancer tend to be at a higher risk of endometrial cancer.
It is important to undertake preventive measures by avoiding the known risk factors when possible. Maintaining a healthy weight, being physically active, controlling diabetes, using oral contraceptives or other forms of hormonal birth control after consulting your gynaecologist, are the best ways to lower the risk of developing endometrial cancer.
Symptoms:
The symptoms include vaginal bleeding after menopause, unusual bleeding between periods, pain in the pelvic area, abnormal vaginal discharge, and pain during intercourse.
Diagnosis:
It is advisable to consult a gynaecologist if you develop symptoms. Based on the symptoms and medical history of the patient, a pelvic examination is performed.
The following tests may also be suggested to confirm the tissue diagnosis:
1. Endometrial Biopsy: It is a commonly performed test. It is done by inserting a very thin, flexible tube into the uterus through the cervix. Suction is then applied to remove a small piece of endometrium tissue through the tube for further examination.
2. Hysteroscopy: A thin instrument with a fibre-optic camera is put inside the uterus for visual examination of the endometrium and a biopsy is taken from the abnormal area.
3. Dilation and curettage (D&C): The sample is collected by dilating the cervix and scraping the tissue from the endometrium with a special tool.
Once the diagnosis is made the following tests may be recommended to know the spread of the disease:
Pelvic examination
TVS/MRI/CT scan/PET CT
Stages:
If not controlled, endometrial cancer tends to spread from the uterus to other parts of the body over time. This cancer is broadly classified into four stages:
Stage 1: At this stage, the cancer cells are only present in the uterus.
Stage 2: Cancer replicates in the uterus and cervix.
Stage 3: Cancer spreads outside the uterus that is in fallopian tubes, ovaries, vagina, and/or nearby lymph nodes.
Stage 4: In the last stage, cancer reaches out to the bladder and rectum and/or spreads beyond the pelvic area to distant tissues and organs.
As with other cancers, endometrial cancer also needs to be treated in the early stages of the condition for the best outcomes.
Treatment options:
1. Surgery is commonly recommended to treat endometrial cancer which involves removing the uterus, ovaries, and fallopian tubes. At times lymph nodes and other tissues may also be removed.
2. Radiation Therapy is used to kill cancer cells by using high-energy beams. It is often performed after surgery to kill the remaining cancer cells and at times as palliative therapy.
3. Chemotherapy involves the use of drugs to kill cancer cells. It is recommended in the later stages of cancer when it has spread to the other parts of the body.
4. Hormone Therapy: Treatment with progestin is an option for women with early-stage slow-growing tumours who want to have children or for women who cannot have surgery because of other medical reasons.
If detected early, endometrial cancer is highly curable. Timely diagnosis needs to be prioritised and encouraged among all women.
The writer is Chairperson, Gynecology and Gynae Oncology, Medanta Hospital.