

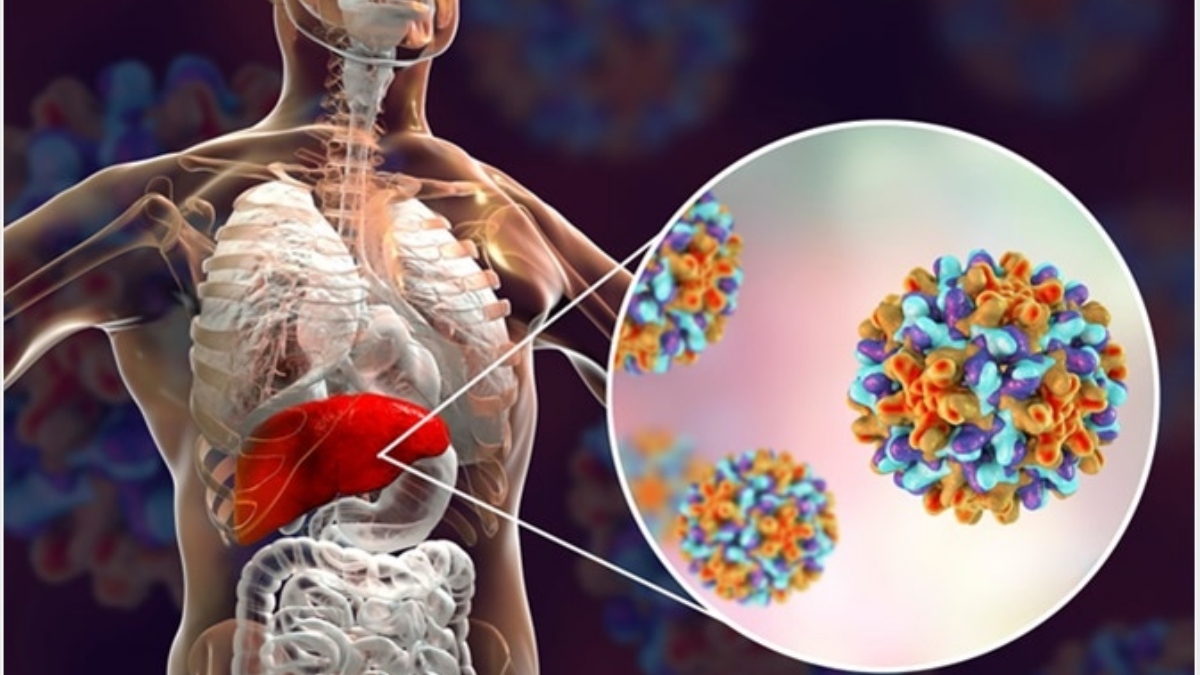
According to the World Health Organization, “Hepatitis B is a potentially life-threatening liver infection caused by the hepatitis B virus (HBV). It is a major global health problem. It can cause chronic infection and puts people at high risk of death from cirrhosis and liver cancer.”
WHO estimates that 296 million people were living with chronic hepatitis B infection in 2019, with 1.5 million new infections each year. World Hepatitis Day takes place every year on 28th July to bring the world together under a single theme to raise awareness of the global burden of hepatitis especially with more focus on viral hepatitis and to influence real change.
To discuss the same we had a panel of experts: Dr Anil Arora, Head of Gastroenterology Dept, Sir Gangaram Hospital; Dr. Sanjiv Saigal, Principal Director, Liver and Hepatology, from Max Chain of Hospitals; Dr Sudeep Khanna, Senior Consultant, Gastroenterology Dept, Apollo Chain of Hospitals.
Question: Dr. Saigal, why is hepatitis such a crucial problem? According to WHO reports a person dies of Hepatitis dies every 30 second.
Dr. Sanjiv Saigal: Hepatitis is a huge burden in our country as it is worldwide. Hepatitis basically means inflammation of the liver ad the prime reason for this are the hepatitis viruses which are of four types primarily: Hepatitis A, Hepatitis B, Hepatitis C, Hepatitis D. Hepatitis A & B are self-limiting and spread through blood, water or any fluid. But Hepatitis C & D are huge burden in our country and spread through parental fluid. In India, Hepatitis B has a prevalence of 2-7% and Hepatitis C is 0.5-1.5%. They constitute a huge number if patients in the county and are very important cause of liver related deaths in the country. They also cause liver failure, liver cancer and so on. Thus, it should be our topmost priority to treat and cure this disease.

Question: 40 million people in India are HBV infected and constitute about 11% of the global rate. What would you say Dr. Arora?
Dr. Arora: This topic is very pertinent as Covid will come and go but the illnesses like Hepatitis have not gone ever since. Certain viruses are spread through contaminated water and infected fluid, which are totally preventable. This is a prevalent issue in developing countries like India and South Asian nations whereas it has been totally eradicated in developed countries. Simple provision of safe drinking water and hygiene can prevent Hepatitis A & E. Virus spread through parental route are problematic. Hepatitis B & C are neglected, and like you said there are 40 million carriers of the infection unaware of the fact that they are infected, hence they are not only potentially disease developers but are also becoming a threat for their families. By increasing awareness, we can prevent this.

Question: Dr. Khanna would you agree with Dr. Arora that there is a problem of awareness that needs to be tackled right away?
Dr. Sudeep Khanna: I would like to add something to it, people know that something like this exists but they are not ready to accept it. A recent study conducted on 1 lakh children from India concluded that only 50% of the children were vaccinated against Hepatitis B.

Question: Isn’t it covered under Universal Health Immunization? Then why aren’t people getting vaccinated?
Dr. Sudeep Khanna: For the same reason as why they wouldn’t get anti-covid vaccine. This becomes a problem for us to help people. The vertical and horizontal transmission from mother to baby and during close contact is the most common cause of Hepatitis B. People need to be tested, treated and educated.
Question: Dr. Arora, we rightly spoke about how people are not even ready to accept it. So what can people do to prevent this stigma?
Dr. Anil Arora: A wonder drug called DAA has been discovered which can cure almost any type of Hepatitis C and hence it is as curable as any other disease but Hepatitis B is problematic. They are not aware of the fact that they may be carrying the virus in their blood for ages before they come down with advanced diseases like Cirrhosis and Carcinoma. My advise will be that anybody with a history of liver transplant, blood transmission, surgery, needle prick trauma or even dental manipulation should get a checkup for Hepatitis B. Now coming to vaccination, Hepatitis B vaccines has been available for over three decade at very low rate and very efficient.
Question: There are about 1.1 million who have died due to Hepatitis, and 3 million are still carrying the disease worldwide. How do we really address this in India especially with the urban rural divide?
Dr. Sudeep Khanna: Multimedia and TV are such a big medium and still unused to their full capacity. A lot of people don’t know about Hepatitis C and lack of initiative from the authorities and doctor bodies are causing this. The disease is significantly asymptomatic and by the time they are symptomatic it is too late. So it is all about awareness.
Question: Dr. Arora, what can one do if one is already infected with Hepatitis B? What about cure?
Dr. Anil Arora: There are two aspects of patient suffering from Hepatitis B, unlike other illnesses, if someone gets an infection today, there are 5% chances that as an adult they will carry the virus in the blood for the next 6 months that is called chronic carrier state and may develop the disease later in life. They remain asymptomatic and thus do not bother about it. This is where screening is needed and if a person is accidentally positive for Hepatitis B, he can be treated with antiviral therapy or else he may spread it to his family. In early diagnosis, regular follow up goes a long way in preventing the chronic illness.
Question: Dr. Saigal, can a patient of Hepatitis B follow up with their checkup if infected with Covid?
Dr. Sanjiv Saigal: Patients ask that if I am Covid positive then what happens with the other problems of mine and if you look at Hepatitis, the patients are consulting specialist doctors, and hence can manage with a teleconsultation and it is not required to come to the hospital. If there is an emergency, then they should visit the hospital no doubt. If a Hepatitis patient is Covid positive and taking the concerned medications, I would recommend that they don’t stop taking medicines for Hepatitis as this may provide a flare to the disease.
Question: Dr. Khanna, are the patients with Hepatitis at a greater risk if they get Covid? Are they furthermore immunosuppressed like we have seen in Cirrhosis?
Dr. Sudeep Khanna: If one has Cirrhosis, they are not at higher risk of getting infected. If in case the liver function goes down, the risk of Covid complication increases. Similarly, being infected with Hepatitis B or C does not mean that you are at higher risk of getting Covid. There should be no fear of vaccination.
Question: Dr. Arora, what would you say on the point “ No fear of vaccination”?
Dr. Anil Arora: Liver is a vital organ in many functions including metabolism and immunity. Once you have severe Covid, liver gets involved in the immunity in many patients. Patients who have underlying liver disease should be given vaccine on a priority basis. Because liver handles all the drugs given to the covid patient.
Question: In what conditions in Covid patients does it lead to diseases like Cirrhosis other complications?
Dr. Sanjiv Saigal: If you develop Jaundice due to contaminated food or water, it is a small chance that they may develop rapid deterioration and altered sensorium thus may have to be admitted to ICU. If someone has chronic disease like Hepatitis B or C and catch infection like Pneumonia, Covid, etc. then they may develop a liver failure. These are the two situation which may cause rapid deterioration and both the type of patients should be diagnosed early and quick treatment can save these patients.
Question: How can the person know that they are carrying the Hepatitis infection?
Dr. Sudeep Khanna: For most of the patients, the disease is asymptomatic. And hence is it not possible for them to diagnose through symptoms. Tiredness, although is a primary symptom so if you have fatigue throughout the day, you may have Hepatitis. One other way is to know if a family member is diagnosed with Hepatitis, one may be a carrier for the disease. Also, screening the high risk population is a way out.
Question: Dr. Arora, we spoke about who all should get tested, what will be your suggestion to all the policy makers?
Dr. Anil Arora: the only way to pick it up early and diagnose is by testing. So my suggestion is that whenever going for any sort of blood test or screening, get tested for Hepatitis B and C. and executive check up is becoming a routine. It should be mandatory and if an asymptomatic patient is not checked up early, the cost of long-term disease treatment is enormous. While it is very cost effective in early stages.
Question: Dr. Saigal, is there anything that we can do to prevent it other than screening or vaccination?
Dr. Sanjiv Saigal: As we discussed, we have to identify the high risk population. We need to look for any family member with Hepatitis. If you have a liver problem, you should get it checked. Then you need to avoid contaminated food and liquid. Be careful in interpersonal relationships. Dialysis and following all protocols strictly may help diagnose and treat Hepatitis. We should follow universal practice of screening people. Be aware and screen people which may help people to curb the disease.
Question: what do you suggest policy makers, institutions and common people to eliminate the disease?
Dr. Sudeep Khanna: As an individual I can only think of vaccine being made mandatory which is very difficult in the democracy. Other than that nothing is going to help.
Since we all go to annual checkups, our panelists suggest that do get checked up for Hepatitis on a routine basis, avoid contaminated food and get proper vaccination.