The recent surge in measles cases across twelve states in the U.S. has triggered concerns among healthcare professionals about the potential resurgence of other vaccine-preventable diseases. As of March 6, 2025, the United States reported 222 measles cases, including one confirmed death, with another fatality under investigation. This outbreak signals possible future outbreaks of diseases such as polio, rubella, and mumps—conditions that were previously under control due to successful vaccination programs.
The Current Measles Outbreak: A Wake-Up Call
Measles, a highly contagious viral disease, serves as a key indicator when vaccination rates decline. According to Dr. Adam Ratner, director of pediatric infectious diseases at NYU Langone and Hassenfeld Children’s Hospital, a drop in vaccination rates first manifests through measles outbreaks. The current numbers—222 cases in approximately two months—nearly match the total for 2024, which stood at 285 cases for the entire year. Texas has been significantly affected, with cases rising to 223 from 159 in just one week.
Measles outbreaks serve as a critical warning signal, highlighting gaps in community immunity and potentially foreshadowing outbreaks of other preventable diseases.
The Importance of Community Immunity
Community immunity, often referred to as herd immunity, requires high vaccination rates to protect the entire population, including those who cannot be vaccinated due to medical reasons. For measles, this threshold is around 95%, according to Dr. George Rust, a professor of medicine and co-director at Vanderbilt University Medical Center. The CDC reported that the vaccination rate for measles for the 2022-2023 school year was 93.1%, slightly below the required threshold. Alarmingly, vaccine exemption rates have risen, with 10 states reporting exemption rates of 5% or higher.
For polio, the community immunity threshold is slightly lower, at about 80%, yet similar concerns about declining vaccination rates exist.
Polio: A Silent Threat Re-Emerging
Polio, a crippling and potentially deadly disease, had been nearly eradicated in most parts of the world thanks to aggressive vaccination campaigns. However, reduced vaccination rates risk reversing these gains. The poliovirus spreads through contaminated food and water and can cause irreversible paralysis.
Dr. George Rust, professor of medicine and co-director at Vanderbilt University, warns that the fear surrounding polio’s return is not unfounded. The U.S. witnessed a small polio outbreak in New York in 2022, underscoring the disease’s latent threat.
To maintain community immunity, the CDC recommends that children receive the inactivated poliovirus vaccine (IPV) at 2 months, 4 months, 6–18 months, and 4-6 years, with a booster in adolescence.
Rubella: The Forgotten Risk
Rubella, or German measles, is another disease under the watchful eye of doctors. Unlike measles, rubella causes milder symptoms but poses a significant risk to pregnant women, where it can lead to congenital rubella syndrome (CRS) in newborns. CRS can result in heart defects, cataracts, deafness, and developmental delays.
Rubella’s near-elimination in the U.S. can be attributed to the widespread use of the MMR (measles, mumps, rubella) vaccine. However, the current measles outbreak raises concerns that rubella cases may follow if vaccination rates continue to decline.
Healthcare experts stress the importance of the MMR vaccine in preventing rubella. Dr. Schaffner emphasizes the need for parents to adhere to vaccination schedules to avoid outbreaks and protect vulnerable populations.
Mumps: A Resilient Adversary
Mumps, caused by a virus that primarily affects the salivary glands, can lead to complications like meningitis, encephalitis, and infertility. Despite the availability of the MMR vaccine, mumps outbreaks occur sporadically, often in close-contact settings like schools and colleges.
Recent years have seen an uptick in mumps cases, raising alarms among doctors. The CDC reports that mumps outbreaks often occur in communities with lower vaccination coverage or during lapses in booster vaccination adherence.
The MMR vaccine effectively prevents mumps, but its efficacy can decrease over time, necessitating booster shots during outbreaks or as part of regular immunization schedules.
Challenges in Maintaining Vaccination Rates
Several factors contribute to declining vaccination rates, including vaccine hesitancy fueled by misinformation, cultural beliefs, and complacency. The COVID-19 pandemic also disrupted routine vaccination schedules, leading to missed doses and gaps in immunity.
Vaccine hesitancy remains a significant barrier. Misinformation about vaccine safety and potential side effects circulates widely on social media platforms, creating confusion among parents and caregivers. Healthcare professionals play a crucial role in addressing these concerns by providing accurate information and reassurances about vaccine safety.
Access to vaccines is another critical issue, particularly in rural or underserved areas. The CDC and public health bodies emphasize the importance of maintaining robust vaccine distribution networks to ensure that all communities have access to life-saving vaccines.
The Role of Public Health Initiatives
Public health authorities must prioritize education and outreach programs to counteract vaccine hesitancy. The CDC’s efforts to promote vaccination through school programs, community engagement, and partnerships with healthcare providers are vital in maintaining high vaccination rates.
Programs like the Vaccines for Children (VFC) program offer free vaccines to eligible children, reducing financial barriers and encouraging timely immunization. Public health campaigns focusing on the importance of vaccines and community immunity can enhance awareness and participation in vaccination programs.
Addressing Misinformation
Misinformation remains a significant barrier to vaccination efforts. Social media platforms are often rife with inaccurate claims about vaccines, leading to fear and reluctance among parents. Healthcare providers and public health officials must actively engage in debunking myths and sharing scientifically backed information.
Dr. Ratner advocates for transparent communication between healthcare providers and parents. “Clear, consistent, and science-based messaging is essential to maintaining trust and ensuring high vaccination rates,” he says.
The Future of Vaccine-Preventable Diseases
The current measles outbreak serves as a stark reminder of the consequences of declining vaccination rates. Doctors and public health officials are urging parents to adhere to vaccination schedules and consult healthcare providers for updated immunization information.
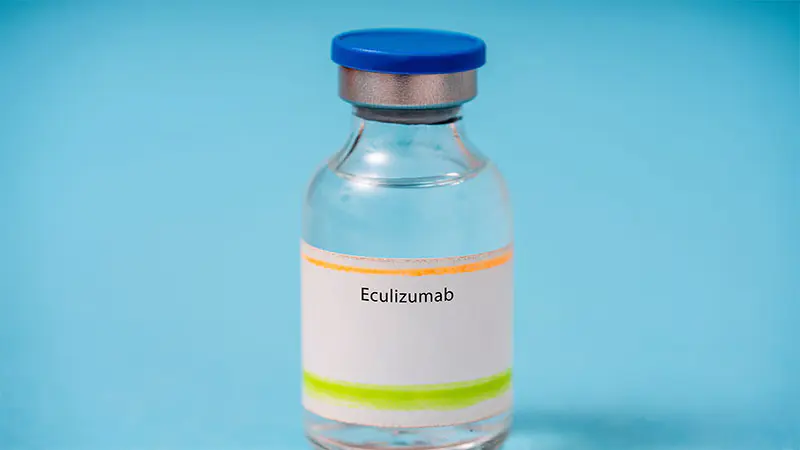
Looking forward, healthcare systems must prioritize research and innovation in vaccine development. New vaccines for diseases like respiratory syncytial virus (RSV), dengue, and COVID-19 variants are under development, highlighting the importance of continuous advancements in immunization science.
Healthcare professionals advocate for policies that ensure vaccine equity, improve access, and reinforce the importance of community immunity. Schools, workplaces, and community organizations play pivotal roles in promoting vaccination and safeguarding public health.