


We must have heard or seen situations like “A 50-year-old man jogging in the park. He suddenly collapses and people in the park surround him” Or “Oh ! he was well last night, I have talked to him, but expired suddenly in the early morning” And we keep wondering what could be the reason!!
Every year, about 4,280 out of one lakh victims of sudden cardiac arrest (SCA) die in India. Sudden cardiac arrest is a condition where the heart stops its function of pumping blood to the whole body leading to the cessation of heartbeat and breathing. The terms cardiac arrest and heart attack are often used interchangeably, but these are two different conditions. A heart attack occurs when an artery is blocked due to fat and cholesterol deposition and prevents blood from reaching the heart muscle causing severe chest pain and breathing difficulty. Whereas cardiac arrest often occurs suddenly without any warning due to disturbance in the electrical activity of the heart that causes an irregular heartbeat (arrhythmia) which disrupts the heart’s ability to pump blood to the brain, lungs, and other vital organs. Disturbance in the electrical activity of the heart leading to cardiac arrest can be due to any of the following reasons: diabetes, hypertension, lungs, liver and kidneys diseases, etc. However, it can happen to anybody at any point in time. Within few minutes of cardiac arrest, the victim becomes unconscious and death occurs within minutes if the victim didn’t receive treatment. It has been observed that “ Every minute’s delay in the resuscitation of the cardiac arrest victim reduces the chance of survival by 7-10%”. So a prompt action can save the person’s life with cardiac arrest.
India is a vast country with lots of diversity, differences in culture, language, religions, customs, atmosphere, socio-economic issues, and differences in terrain. The environment and the infrastructure for resuscitation of a person with sudden cardiac arrest vary from place to place. So there was a need for a structured guideline to be followed for resuscitation of cardiac arrested victims. Moreover, the approach should be such that it is applicable at all scenarios and remains scientifically valid. There is a large body of evidence to show that it is possible to save the victims of SCA with immediate high-quality bystander hands-only cardiopulmonary resuscitation (CPR) – Compression only life support (COLS)
Compression only life support (COLS) are the guidelines developed by the Indian Resuscitation Council for providing only chest compressions in a stepwise algorithmic approach by a layperson for the cardiac arrest victims till the time medical help arrives
The timely management of the victim with cardiopulmonary arrest is paramount. It may not be possible to provide immediate medical care by the trained person when the victim is outside the hospital. The inclusion of common man after their proper training would be beneficial to improve the outcome of the victim. However, the medical steps to be taught to a layperson should be kept simple and easy to follow, and yet evidence-based.
Learning the skill of saving one’s life is may not be easy. But it is equally not easy to ignore someone dying unattended. Let us all try and make a world where no one dies from cardiac arrest. The Compression only Life Support (COLS) provides an easy, algorithmic stepwise approach for resuscitation of the victim with cardiopulmonary arrest by the lay person. To save one’s life, you should know various steps of COLS-Compression Only Life Support.
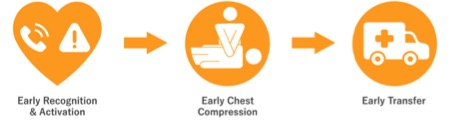
The main activity of Compression-Only Life Support (COLS) is effective chest compression which should be performed continuously till help arrives. The chest compressions are performed at the rate of 120 per minute and the depth of each chest compressions should be around 5-6 cms.

To enhance the outcomes in cardiac arrests we need high-quality adult resuscitation education and Hands-on Training to maximum citizens. To achieve this, we first need to create the awareness and creating confidence among laypersons, that their contribution is equally important for the survival of a sudden cardiac arrested victim outside the hospital.
The main motto of any project related to layperson training in CPR is to bring out wide popularity for resuscitation, impart training to as many laymen including school children so that every citizen becomes a lifesaver. The IRC aims to train at least one person in the family to save the life from sudden cardiac arrest.
So, remember, Each of one us can save a life. Your two hands can save a life. Your timely help with compression-only CPR (COLS), in this emergency, may save somebody’s life. This victim could be your family member, friend, or a stranger on the street! Let us take a pledge on this National CPR day to learn CPR.
About the authors: