

Today is July 1 and every year this day is observed as National Doctors’ Day in India to express gratitude and acknowledge the dedication and commitment of the doctors’ towards our society. The observance of the day honours legendary physician and West Bengal’s second Chief Minister, Dr. Bidhan Chandra Roy whose birth and death anniversary coincides on the same day. As we continue to fight the second wave of the pandemic and prepare ourselves to beat the third wave, as a practicing neonatologist, I am deeply concerned about two issues that still continue to affect the medical fraternity i.e. physician burnout amidst the ongoing pandemic and violence against doctors adding insult to the injury.
I have always been debating and seeking answers to the question at several forums “why always only doctors are answerable to the society”. Most often and almost regularly for any incident that relates to the health and wealth of the society, a doctor is responsible and straightway it is termed as medical negligence? Why? Are we trying to say other professions like judiciary, administration, banking and so on do not have any negligence? Our doctors, nurses, carers and paramedics around the world are facing an unprecedented workload in overstretched health facilities, and with no end in sight.
WHY THE BURNOUT?
“Please, please wear masks. I don’t know about other people but I’m physically and mentally exhausted with crazy shifts and calling more deaths than I did in all my years of service combined,” reads a tweet by Dipshikha Ghosh, a doctor in critical care medicine, per her Twitter bio.
Mounting deaths, long hours, low pay, lack of resources, and the risk of contracting COVID-19, India’s healthcare workers are facing a mental health crisis. The stress of long hours, no sleep, poor eating, inadequate protection, the fear of contaminating loved ones, the fear of dying and seeing patients die no matter what you do, the disrespect by hospital administrators and the fear of being fired, all remain the reality for those who are in the thick of things. Adding to this, the junior doctors have been in the limbo for over a year – without qualifying, but working and expected to work as doctors – without proper pay as doctors – all adding to the burnout even befoVre they start their career. Physician burnout costs the United States healthcare industry $4.6 billion a year – a number that was pre-pandemic and during the pandemic it was expected to have costed double this. No such estimates are known for India. While burnout is increasingly being recognized globally as a major concern, affecting physical and mental well-being of HCWs, with the current pandemic, closing down of international and state borders, strict city, and also area wise lockdown has affected HCWs and their families as well, causing excessive negative psychological effects. Besides, negative consequences for the physicians, and patients, and the health-care system, available data also suggests that it is important to recognize burnout at the earliest and use preventive strategies for emergence of the same. Many people have lost their loved ones to COVID including healthcare workers & their families. There are times when people blame their doctors for their loss. If this was true, then no doctor or their family members would have lived forever. However, no one considers the physical and mental stress of the doctors while fighting new strains.
India needs to have clear-cut guidelines for the management of burnout which is currently missing. Some of the individual-level interventions, which are thought to be helpful for burnout should be practiced such as cognitive-behavioral techniques, meditation and relaxation techniques, development of interpersonal skills, and development of knowledge, work-related skills and proper recognition & appreciation of their work. In addition to this, various interventions carried out at the level of organization and the physician–organization interface should be proposed to address physician burnout. It is important to understand that when patients were left to fend for themselves by relatives, it was doctors and nurses who risked their lives for them. We need to have a national study on the mental state of healthcare workers especially during this pandemic which will be a proof that our healthcare workers are overworked and those who took COVID duty also found themselves without enough sleep.
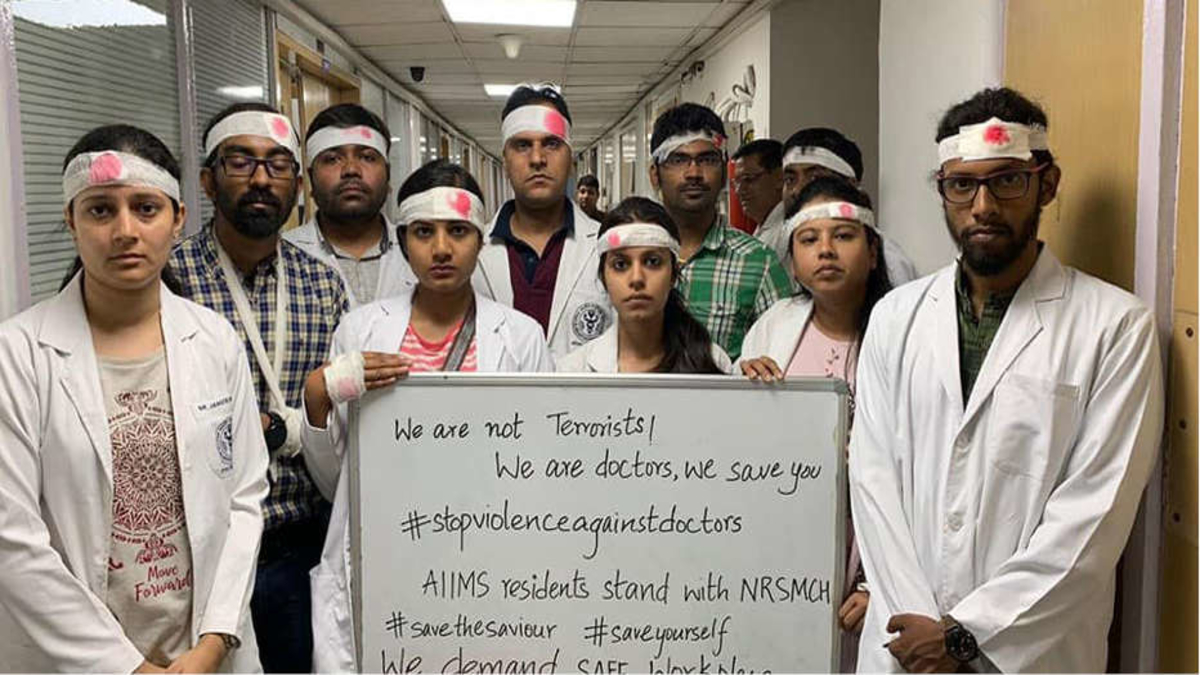
Violence against Doctors: Growing epidemic?
Recently, an on-duty doctor was attacked by a policeman in Kerala. Doctors serving in COVID wards have been beaten and brutally assaulted in Bihar, West Bengal, Assam, Uttar Pradesh, and Karnataka. Just few weeks ago, a Pediatrician was attacked in Tarikere and a intensive care physician was attacked in Bangalore private tertiary hospital. There have been numerous incidents highlighting violence inflicted on the healthcare staff. Over 80% of doctors in the country are stressed and 75% of doctors deal with abuse and assault, as per an IMA report. What may seem like impulsive outbursts of violence by patients or their attendants against doctors actually points to the chronic neglect of public health by the Indian state?
Workplace violence against doctors is not new, but in recent times, it has grown up in epidemic proportions. Doctors are more worried about their safety and life in the workplace. Meager government spending on healthcare associated with the poor socioeconomic status of the patient and the ever-rising cost of treatment had worsened the situation in present times.
Healthcare in India is complicated, spanning across acute care, preventive and public health. And private healthcare delivers nearly 80 per cent of the country’s needs. But doctors in both public and private sectors are at the receiving end of violence. The public sector is in general blamed for most of the faults of the services sector.
In a land where swamis and soothsayers make more television appearances than doctors, society needs a strong medical role model. Hospitals need to improve its services on par with global standards and ensure that enough doctors and para medical staff are employed to handle patients. We need to see a change in government policies like increased government spending on healthcare, improving the infrastructure of the hospitals, stricter implementation of rules, laws, and punishment for violence under the Prevention of Violence against Doctors and Hospitals according to appropriate Acts and relevant sections of the Indian Penal Code (IPC), violence against health-care personnel and hospitals should be made a non bailable offense and damages should be recovered from the persons responsible for the violence. The government should take responsibility for the safety of healthcare workers. Australia had a spike of violence against healthcare workers in late 1990s & early 2000s, immediately the government reacted and introduced 12 years imprisonment for any person convicted of violence against healthcare workers. Soon the violence against them virtually disappeared. Clearly it shows that only stricter imposition of the rules & law enforcements can save the profession and professionals.
In addition, all institutions should have a standard operating procedure and code purple should be declared and all measures should be taken in case of violence. Security staff to respond and assist immediately.
Patient awareness is the key. Patients need to be educated and be informed that doctors practice medicine and they cannot be held responsible for every death occurring in the hospital on the ground of negligence. Cost increases with the type of treatment & its advancement. Our medical schools, along with the medical subjects they should also teach about patient-doctor relations, communication with the patient in an effective way, empathy towards the patients and their relatives. The school should also teach them how to handle tactfully when the patients or their relatives behave aggressively and the situation turns chaotic and violent. They should teach them how to remain calm and responsible during those times without compromising the quality of patient care as well as safety.
Unless there is an entire overhaul of the prevailing healthcare system& a political will to protect the healthcare workers, it is a herculean task to curb violence against doctors, which will be a disaster much worse than covid-19.
The Author is the Founder Chairman & Neonatologist, Cloudnine Group of Hospitals, Bengaluru. Author is also a healthcare delivery graduate from Harvard Business School