

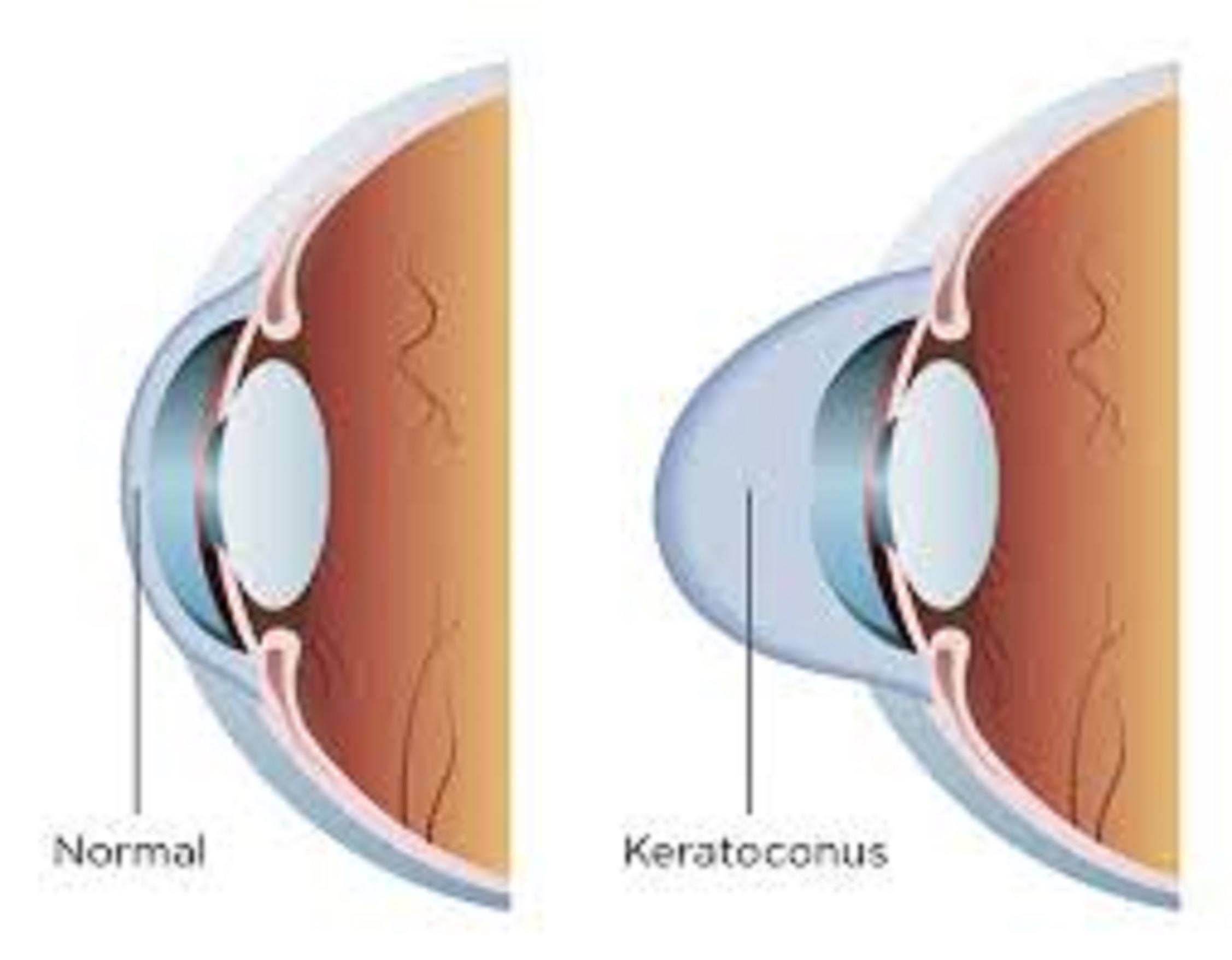
Keratoconusis is a phenomenon that occurs when your cornea, i.e., the clear, domeshaped front surface of your eye, thins and gradually bulges outward into a cone shape. This causes blurred vision and sensitivity to light and glare. The ailment usually impacts both eyes, though it often impacts one eye more than the other. Keratoconus is not a common condition. It happens more often in young adults in their teens and twenties. It affects men and women in equal numbers.
SYMPTOMS
The signs and symptoms of keratoconus may change as the disease progresses. They include: – Blurred or distorted vision
– Need to frequently changes eyeglasses
– Sudden worsening or clouding of vision
– Heightened sensitivity to bright light and glare, which can cause problems with night driving
– It is important to see your eye doctor (ophthalmologist) if your eyesight is worsening rapidly, which might be caused by an irregular curvature of the eye (astigmatism). You can also look out for signs of keratoconus during routine eye exams.
CAUSES
It is not very clear what causes keratoconus, although genetic and environmental factors are thought to be the causes. Around 1 in 10 people with keratoconus have a parent with the condition. Having a family history of keratoconus, rubbing your eyes vigorously, and having certain conditions such as retinitis pigmentosa, Down syndrome, and asthma are said to be risk factors for keratoconus.
DIAGNOSIS
Your eye care specialist will ask about your health history and give you an eye exam. The doctor will test the sharpness of your vision, and your eyes may be dilated for part of the exam. Your specialist will give you eye drops that widen (dilate) the dark part in the centre of your eye (pupil). This lets your provider see more of your eye more clearly. Your provider may also use a device to measure the curvature of your cornea. Early stages of keratoconus may not be found unless your eye care provider is looking for signs of the disease. An imaging test called corneal topography may help your provider make the diagnosis. This test shows changes in the shape of the cornea.
PREVENTION –
– Protecting your eyes from UV radiation with sunglasses
– Making sure your contact lenses fit well
– Getting treatment for any kind of eye discomfort (for example, from allergies)
– Not rubbing your eyes – Call eye doctor if you have sudden vision loss or sudden pain in your eye
TREATMENT
If you have been diagnosed with keratoconus, the most important thing to do is prevent the condition from worsening and follow the advice of your eye doctor on the best treatment options and follow-up care.
– Depending on the specific characteristics of your keratoconus, these treatment options may include being fitted with scleral contact lenses, undergoing a corneal cross-linking procedure, or both. It’s also very important that you refrain from rubbing your eyes. Eye rubbing has been associated with keratoconus getting worse.
– Successful management of keratoconus requires frequent and lifelong eye exams to make sure your cornea remains stable and your visual acuity is maintained.
– If your keratoconus is progressing, corneal collagen cross-linking might be indicated to slow or stop the progression. This is a newer treatment that has the potential to prevent you from needing a cornea transplant in the future.
– Improving your vision depends on the severity of keratoconus. Mild to moderate keratoconus can be treated with eyeglasses or contact lenses. This will likely be a long-term treatment, especially if your cornea becomes stable with time or from cross-linking.
– In some people with keratoconus, the cornea becomes scarred with advanced disease or wearing contact lenses becomes difficult. In these people, cornea transplant surgery might be necessary. If you are confused or uncertain about the advice you receive from your eye doctor about managing your keratoconus, consider seeking a second opinion from an ophthalmologist who is a keratoconus specialist.
Dr Anand Balasubramaniam is a senior Consultant of Cornea, Cataract and Refractive Services at Sankara Eye Hospital in Bengaluru.